Cell:新分子逆转“衰老”,未发现任何明显副作用
2017-03-25 Chen 生物探索
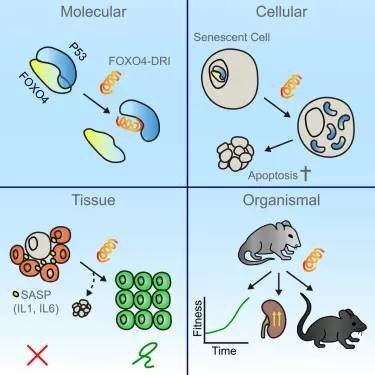
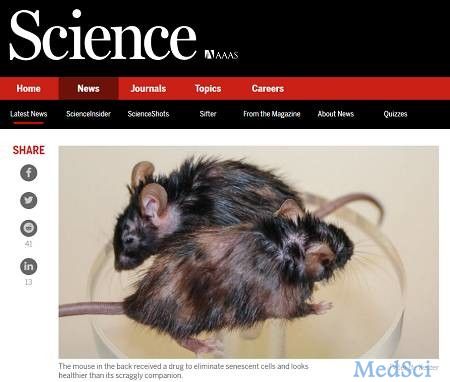
Cell杂志上发表了一篇题为“Targeted Apoptosis of Senescent Cells Restores Tissue Homeostasis in Response to Chemotoxicity and Aging”的抗衰老突破进展。来自荷兰的一个科学家小组发现,定期注射一种肽分子能够选择性地找到并摧毁衰老细胞(senescent cell)。这一结果为改善自然衰老小鼠以及

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Cell#
103
#副作用#
50
#新分子#
68
#CEL#
66
不错,学习了
149
牛
107
看好这个研究前景
0