NEJM:Paget骨病-案例报道
2016-04-01 chensuo译 MedSci原创
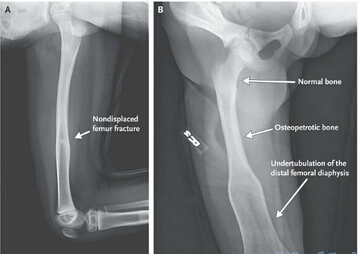
男性,57岁,近来右膝和右大腿部出现严重的皮温上升和肿胀,导致其感到剧烈的疼痛。 常规体格检查发现右大腿与与左腿相比,关节运动可见明显的不对称。 X线检查显示骨性肿大和皮质增厚(如图A箭头所指处),右髂骨的骨小梁和股骨延长至软骨下区部分明显增粗(如图A和B,黑色箭头处),与双侧髂耻增厚(如图B,箭头处)和坐骨线(如图B,白色箭头处)。 以上所有的这些检查结果都与佩吉特骨病的症
男性,57岁,近来右膝和右大腿部出现严重的皮温上升和肿胀,导致剧烈疼痛。

常规体格检查发现右大腿与与左腿相比,关节运动可见明显的不对称。
X线检查显示骨性肿大和皮质增厚(如图A箭头所指处),右髂骨的骨小梁和股骨延长至软骨下区部分明显增粗(如图A和B,黑色箭头处),双侧髂耻增厚(如图B,箭头处)和出现髂坐线(如图B,白色箭头处)。
以上所有的这些检查结果都与 Paget骨病的症状完全相符。
此外,双侧髋关节软骨存在明显畸形,左股骨近端可见明显毛刺样病变(如图B,红色箭头处)。
实验室检查发现骨中碱性磷酸酶水平位32μg(正常为<20μg)。骨扫描显示病变骨部位异常严重(如图C)。
最后,该患者接受利塞膦酸钠药物进行治疗。
18个月后对其进行随访,其表现的症状明显减少,骨扫描结果可见其病变骨部位明显改善(如图D)。
原始出处:
Ankit Balani, M.B., B.S., and Sapna S. Marda, M.B., B.S., M.D. Paget’s Disease of Bone,N Engl J Med 2016; 374:1264March 31, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









不错哦,会学到很多
104
好文,值得学习,赞!
92
#Paget#
84
骨科为什么出现到普外科
172
值得学习 谢谢
148
解释详细
165