Cell:要想记忆好 睡眠不可少
2015-06-16 佚名 生物谷
近日,来自佛罗里达的Scripps研究所(TSRI)的研究人员们发现,睡眠可以抑制一些促进遗忘的神经细胞的活性,从而确保记忆得以保存。此项研究在线发表于Cell杂志上。 早前的研究认为,睡眠促进了记忆的保留,这个过程是通过阻止了一些来源于心理和行为活动的干扰。也就是说,睡眠可以将大脑与所有可以干扰记忆储存的刺激隔离开来。而此项最新的研究证明,睡眠促进记忆力保留是通过提高巩固记忆的能力。
近日,来自佛罗里达的Scripps研究所(TSRI)的研究人员们发现,睡眠可以抑制一些促进遗忘的神经细胞的活性,从而确保记忆得以保存。此项研究在线发表于Cell杂志上。
早前的研究认为,睡眠促进了记忆的保留,这个过程是通过阻止了一些来源于心理和行为活动的干扰。也就是说,睡眠可以将大脑与所有可以干扰记忆储存的刺激隔离开来。而此项最新的研究证明,睡眠促进记忆力保留是通过提高巩固记忆的能力。
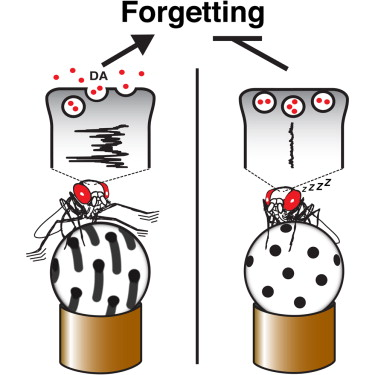
研究人员们利用果蝇作为动物实验模型,他们发现了早前研究的生物学基础,即神经递质多巴胺的活性。多巴胺的活性可以调节多种"可塑性",例如,大脑学习和记忆的能力,及遗忘的能力。研究发现,用促进睡眠的药物Gaboxadol,或者是利用遗传方式刺激睡眠的神经回路,来增加睡眠,均可以降低多巴胺的信号活性,同时可以提高记忆力。反过来,如果增加清醒状态,刺激多巴胺的信号,则可以加速遗忘过程。这种信号活性不是一成不变的,而是与动物的清醒状态紧密相关。
研究人员们表示,睡眠对记忆保留及遗忘的能力,可能是同时进行的,而且是互不干扰的;也有可能更为复杂,有一系列的先后顺序,例如,先有遗忘能力的下降,接着是记忆能力的提高。
通过此项研究,科学家们发现了睡眠可以保护记忆的一种方式,即通过抑制可引起遗忘的多巴胺的神经活性。由于动物和人类均需要睡眠,且均有许多学习和记忆的基因和神经回路机制,所以,在果蝇动物模型上的发现,可以为研究人类睡眠与记忆的关系,提供有用的理论基础。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
65
#CEL#
95
看看
6
有益
157