Cardiovasc Diabetol:有DM的中度冠脉狭窄患者的预后比无DM的重度冠脉狭窄患者的预后更差!
2021-10-26 Nebula MedSci原创
与无糖尿病的重度冠状动脉狭窄患者相比,有糖尿病的中度冠状动脉狭窄患者的预后更差
2 型糖尿病 (DM) 是心血管疾病的主要危险因素。与没有糖尿病的患者相比,糖尿病患者的心血管死亡率增加了两倍以上。既往研究表明,DM 患者的心血管结局也更差,特别是合并冠状动脉疾病(CAD)的患者。
但是,迄今为止,对于患有轻度至中度冠状动脉狭窄 (CAS) 的糖尿病患者的长期预后仍知之甚少。本研究旨在评估冠状动脉狭窄严重程度不同的糖尿病患者的临床结局。
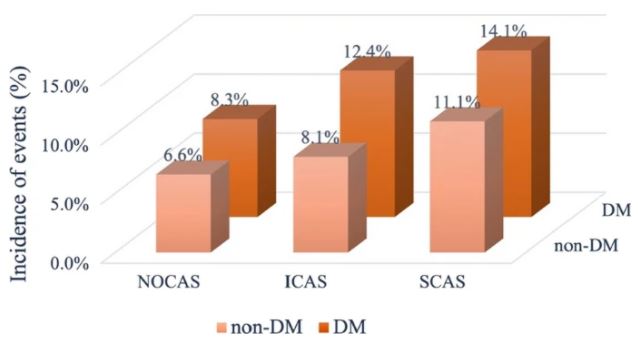
分组情况
该研究连续招募了10,940位因心绞痛样胸痛住院并随访了包括心源性死亡、心肌梗死、缺血性卒中、未计划的冠脉重建和心绞痛相关住院在内的主要不良心血管事件 (MACE) 的患者。根据冠状动脉造影,受试患者被分成了非阻塞性 CAS(NOCAS,狭窄<50%)、中度 CAS(ICAS,狭窄 50-69%)和重度 CAS(SCAS,狭窄 70-100%)亚组,并根据有无合并糖尿病将三个亚组进一步分成了六个小组。
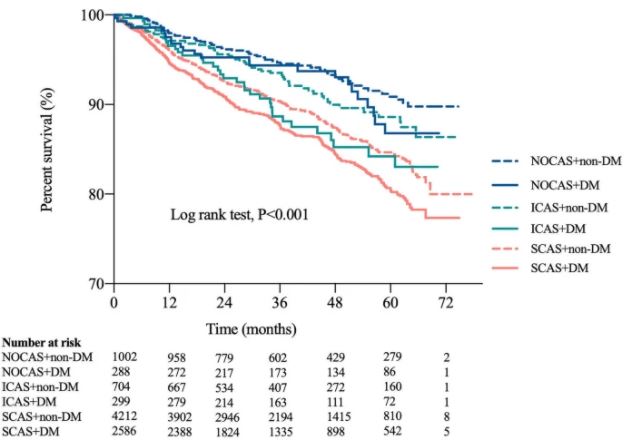
各组患者的Kaplan-Meier曲线
中位随访了40个月,共发生了1017例(11.1%)主要不良心血管事件。在 ICAS 或 SCAS 患者中,合并糖尿病时主要不良心血管事件的发生率会更高(p<0.05)。在亚组分析中,与无糖尿病的 NOCAS 患者相比,有糖尿病的 ICAS 患者、无糖尿病的 SCAS 患者以及有糖尿病的 SCAS 患者的主要不良心血管事件的风险均升高(校正风险比[HR]分别是 1.709[p=0.016]、1.911[p<0.001] 和 2.053[p<0.001])。此外,Kaplan-Meier 曲线分析也显示,有糖尿病的 SCAS 患者发生主要不良心血管事件的风险高于其他人。
总而言之,无论有无合并糖尿病,重度冠状动脉狭窄患者的预后均较差,但与无糖尿病的重度冠状动脉狭窄患者相比,有糖尿病的中度冠状动脉狭窄患者的预后更差。
原始出处:
Zhang, HW., Jin, JL., Cao, YX. et al. Association of diabetes mellitus with clinical outcomes in patients with different coronary artery stenosis. Cardiovasc Diabetol 20, 214 (2021). https://doi.org/10.1186/s12933-021-01403-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BET#
80
#ASC#
94
#DIA#
80
受益匪浅
99
已拜读,受益匪浅。
108
#冠脉狭窄#
83
学习一下
0