年度成就得主马骏教授:手把手教你发NEJM:CSCO2019
2019-09-21 不详 MedSci原创
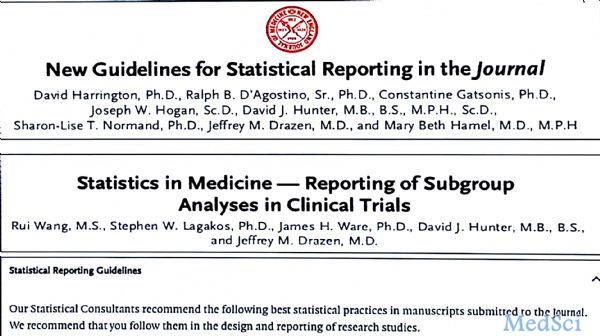
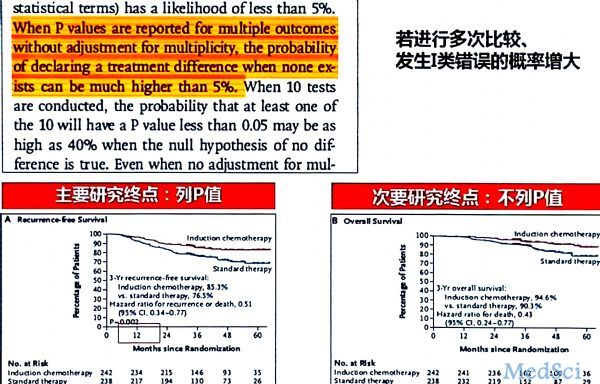
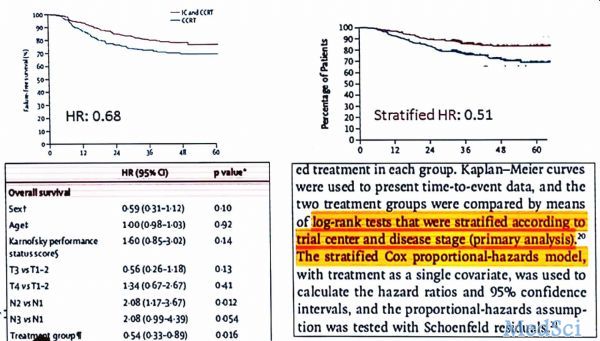
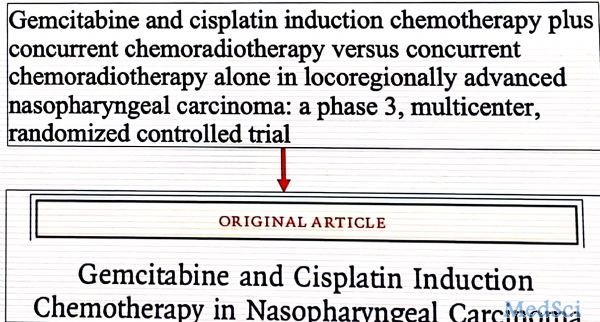
第22届全国临床肿瘤学大会暨2019年CSCO学术年会于9月19日开幕,本届大会将2019年度成就奖颁发给了中山大学肿瘤防治中心 马骏教授 团队的“在局部晚期鼻咽癌患者中,同期放化疗前,吉西他滨+顺铂诱导化疗的III期、多中心、随机对照研究”。此次获奖研究内容发表于新英格兰医学期刊 (The New England Journal of Medicine;简称NEJM)杂志,同时也被选为2019年
.png)


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




.png)











学习学习
106
#马骏#
92
#马骏教授#
69
学习了,谢谢分享
137
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
85