Experi Biol Med:利用母体血清鉴定唐式症相关之蛋白质
2012-06-17 EurekAlert! EurekAlert!
目前使用之唐氏症产前筛检仍待进一步之改进与发展。妇产医学专家正积极投入心力寻找可作为唐氏症筛检之生物标志。来自江苏大学及漳州妇幼医院的邵世和博士与其共同研究者在2012年5月的《实验生物医学》Experimental Biology and Medicine期刊中,发表了他们利用蛋白体学方法在怀有唐氏症胎儿的母体血清中鉴定出29个与唐氏症相关的蛋白质。这些蛋白质除了有可能可以增进唐氏症筛检的正确性
目前使用之唐氏症产前筛检仍待进一步之改进与发展。妇产医学专家正积极投入心力寻找可作为唐氏症筛检之生物标志。来自江苏大学及漳州妇幼医院的邵世和博士与其共同研究者在2012年5月的《实验生物医学》Experimental Biology and Medicine期刊中,发表了他们利用蛋白体学方法在怀有唐氏症胎儿的母体血清中鉴定出29个与唐氏症相关的蛋白质。这些蛋白质除了有可能可以增进唐氏症筛检的正确性外,他们在唐氏症致病机转中可能也扮演了某些重要的角色。
邵博士指出,截至目前为止,对于母体血清中唐氏症相关生物标志的研究仍非常有限。我们目前成功地于母体血清中鉴定出众多的唐氏症生物标志蛋白。
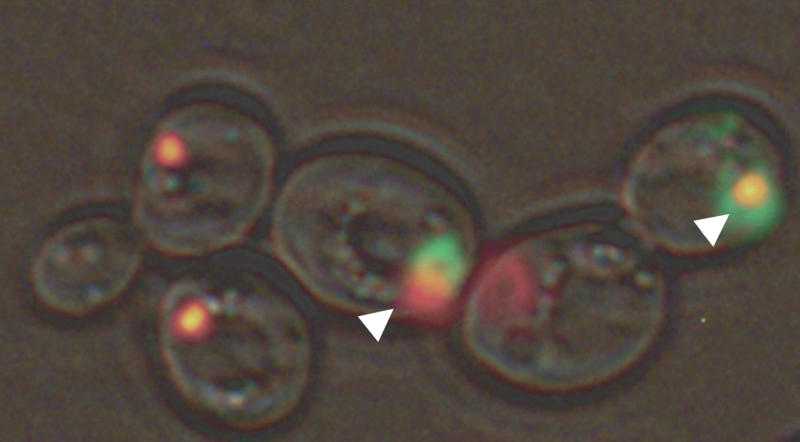
游博士指出,于本研究中我们利用蛋白质体学实验方法中的二维胶体电泳以及基质辅助脱附质谱仪的方法,实验结果证实这些方法有助于鉴定血清中之唐氏症相关的生物标志。
王博士指出,在29个蛋白质当中,以运铜蛋白及补体蛋白乙最值得注意。这两个蛋白质皆于怀有唐氏症胎儿的母体血清中显著的增加。进一步的功能分析更暗示了这两个蛋白质可能与唐氏症的疾病发展有密切的关联。
这些有差异性表现的蛋白质虽然可以提供进一步改进唐氏症产前筛检的机会,邵博士亦指出了目前的研究成果仍有待进一步的临床证实并且他们也将进一步研究这些蛋白质于唐氏症致病机转中所扮演的角色。
《实验生物医学》期刊主编古德曼博士指出,唐氏症产前筛检的诊断准确率约为百分之75至85,伪阳性比率约为百分之5,而在发展中国家中的诊断准确率相对而言就比较低。邵博士及其研究伙伴利用蛋白质体学的方法鉴定出了唐氏症的生物标志,预期将有助于提高诊断准确率及降低伪阳性的比例。(生物谷Bioon.com)

doi:10.1258/ebm.2012.011312
PMC:
PMID:
Preliminary proteomic-based identification of a novel protein for Down's syndrome in maternal serum
Bin Yu1,2, Bin Zhang2, Jing Wang2, Qiu-wei Wang2, Rui-ping Huang2, Yu-qi Yang2 and Shi-he Shao1
Prenatal screening for Down's syndrome (DS) is in need of improvement. As a powerful platform, proteomics techniques could also be used for identification of new biomarkers for DS screening. In this case-control proteome study, pregnant women were diagnosed prenatally by karyotype analysis from amniotic fluid (AF). Maternal serum samples were collected from six pregnancies with fetuses affected by DS and six pregnancies with normal fetuses. First, we used two-dimensional electrophoresis and mass spectrometry to identify the different levels of expression of proteins in maternal serum between the DS and control groups in the second trimester. Second, we used bioinformatics to analyze the proteins by DAVID. Then, the interesting candidates were further tested by enzyme-linked immunosorbent assay (ELISA). Twenty-nine proteins were successfully identified in maternal serum obtained from pregnancies with fetuses affected by DS. The top five proteins up-regulated were serotransferrin (TF), alpha-1b-glycoprotein (A1BG), desmin (DES), alpha-1-antitrypsin (SERPINA1) and ceruloplasmin (CP), while serum amyloid P-component (APCS) was the most down-regulated protein. These 29 proteins were categorized based on binding, catalytic activity and enzyme regulator activity. The biological roles were involved in biological regulation, metabolic processes, cellular processes and response to a stimulus. Based on ELISA, the median concentrations of CP and complement factor B (CFB) were 332.3 and 412.3 ng/mL, respectively. The concentrations of CP and CFB were significantly higher in the DS group than in the control group (P < 0.05). In conclusion, proteomic approaches offer the possibility of further improving the performance of DS screening and our identification of up- and down-regulated proteins may lead to new candidates for DS screening.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
64
#Biol#
56
#Bio#
54
#白质#
68
#蛋白质#
71
#Med#
50