ASCO GI 2020:Zanidatamab在经过治疗的HER2+胃食管腺癌患者中显示出持久的抗肿瘤活性
2021-01-21 Allan MedSci原创
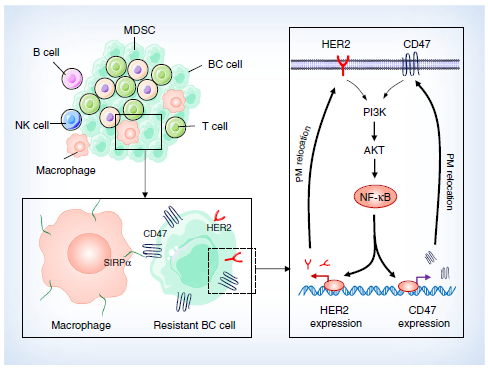
Zanidatamab是一种针对HER2的双特异性抗体。它同时结合了HER2细胞外域IV上的2个不同位点。这种独特的结合导致多种作用机制
在ASCO GI 2020会议上发表的研究表明,Zanidatamab既可作为单一药物,也可与化学疗法联用,在经过治疗的人表皮生长因子受体2(HER2)阳性的胃食管腺癌患者中具有良好的耐受性和抗肿瘤活性。
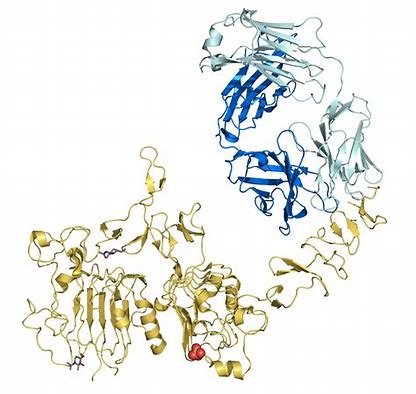
德克萨斯大学安德森分校癌症中心的Funda Meric-Bernstam博士解释说:“Zanidatamab是一种针对HER2的双特异性抗体。它同时结合了HER2细胞外域IV上的2个不同位点。这种独特的结合导致多种作用机制”。
在I期研究的第1部分和第2部分中,患者接受了zanidatamab单药治疗(n = 36),在研究的第3部分中,患者接受了zanidatamab联合紫杉醇或卡培他滨的治疗(n = 26)。大多数患者先前接受过包括曲妥珠单抗在内的至少2种全身性治疗方案。
Meric-Bernstam博士说:“总的来说,仅使用单一疗法,客观缓解率为33%,疾病控制率为61%,反应持续时间为6个月。在接受zanidatamab联合紫杉醇或卡培他滨治疗的患者中,客观缓解率分别为50%和57%,疾病控制率分别为90%和71%。反应持续时间分别为9个月和5.8个月”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#ASC#
68
#胃食管#
65
#肿瘤活性#
73
#食管腺#
90
#抗肿瘤活性#
74
#mAb#
63
#食管#
60
#ATA#
60
#食管腺癌#
81