Stroke: ICH后白细胞升高与血肿扩大减少相关
2016-07-24 phylis 译 MedSci原创
背景:急性白细胞增多是急性脑出血(ICH)的一种反应。白细胞,因为它们与血小板和凝血因子的相互作用,可能会在止血中发挥作用。研究者调查入院白细胞增多是否与急性脑出血后出血减少相关。方法:前瞻性收集从1994至2015原发性脑出血的患者,对其进行回顾性分析。研究包括随访中的CT扫描和症状开始后48小时内的白细胞计数。应用半自动软件计算基线和随访中的血肿体积,血肿扩大定义为体积增大>30%或6mL。应
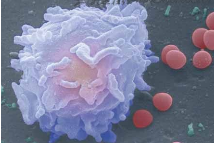
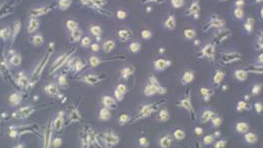
背景:急性白细胞增多是急性脑出血(ICH)的一种反应。白细胞,因为它们与血小板和凝血因子的相互作用,可能会在止血中发挥作用。研究者调查入院白细胞增多是否与急性脑出血后出血减少相关。
方法:前瞻性收集从1994至2015原发性脑出血的患者,对其进行回顾性分析。研究包括随访中的CT扫描和症状开始后48小时内的白细胞计数。应用半自动软件计算基线和随访中的血肿体积,血肿扩大定义为体积增大>30%或6mL。应用多因素Logistic回归分析调查血白细胞计数与脑出血血肿扩大的相关性。
结果:共有1302名受试者符合资格标准(平均年龄为75岁;55.8%为男性),其中207例(15.9%)有血肿扩大。入院时高白细胞计数与血肿扩大风险减少相关(每增加1000细胞的OR : 0.91;95%CI,0.86-0.96)。血肿扩大的风险与中性粒细胞计数呈负相关(OR,0.90;95%CI,0.85-0.96;P = 0.001),和单核细胞计数直接相关(OR,2.71;95%CI,1.08-6.83;)。淋巴细胞计数和ICH血肿扩大没有明显相关性(OR,0.96;95%CI,0.79-1.17)。
结论:较高的入院白血细胞计数与血肿扩张的风险较低相关。研究结果强调急性ICH后,炎症反应在调节凝血级联反应中的作用。
原始出处:
Morotti A, Phuah CL, et al. Leukocyte Count and Intracerebral Hemorrhage Expansion. Stroke. 2016 Jun.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血肿扩大#
84
好文,值得推荐。
113
#ICH#
68
#血肿#
69