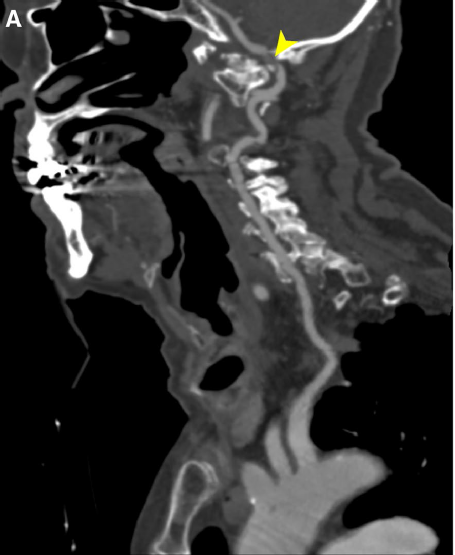
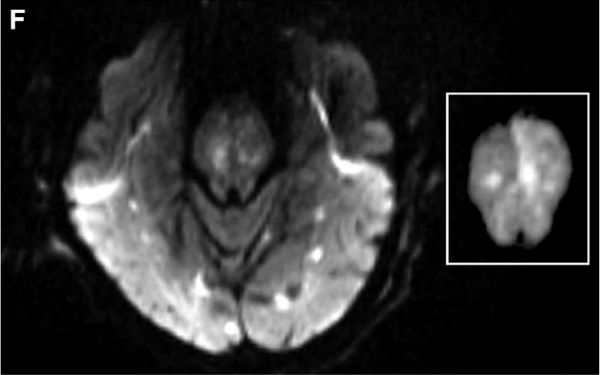
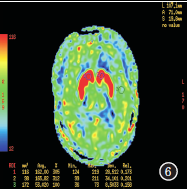
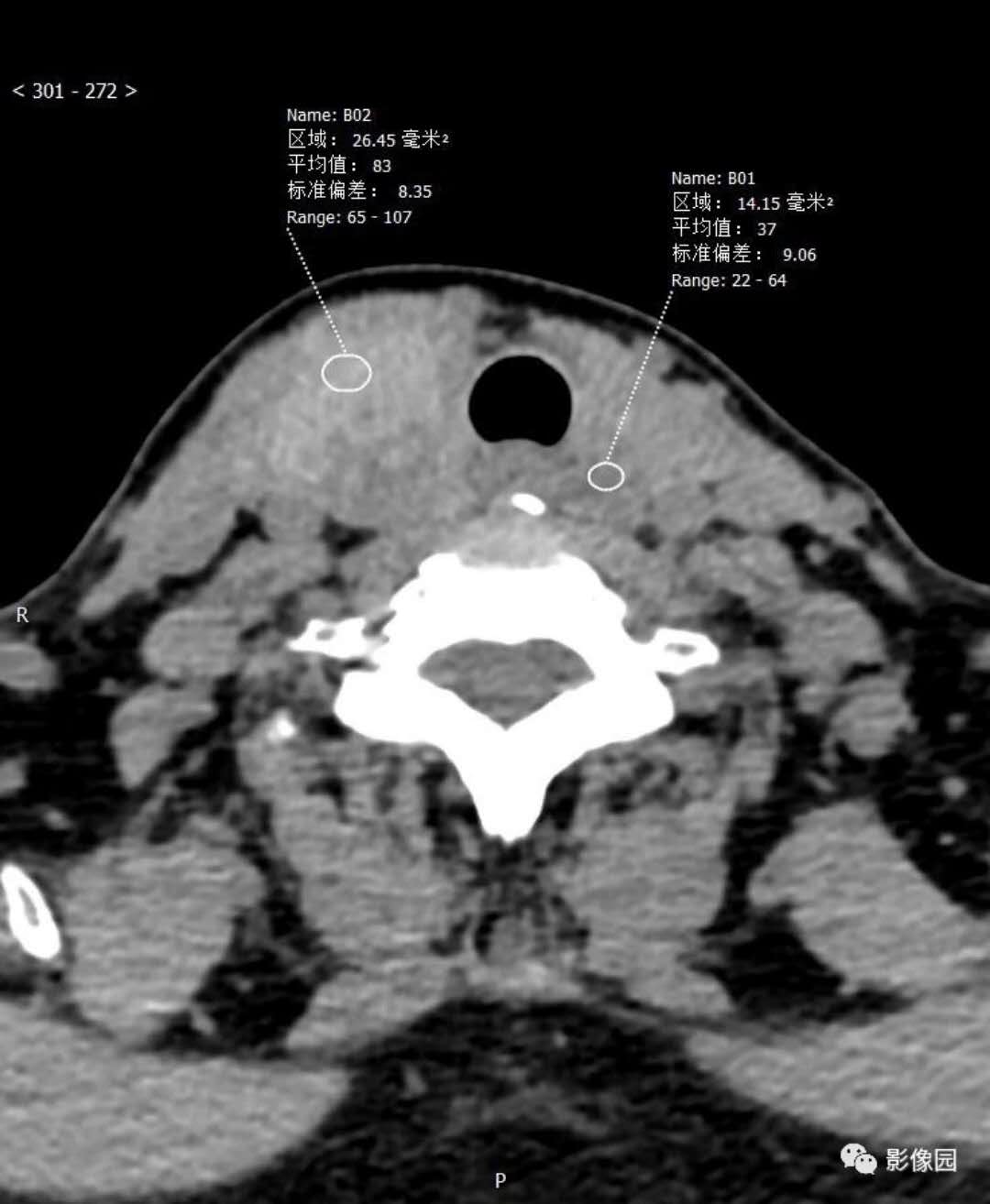
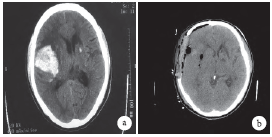
[重复]罕见双侧Bow Hunter综合征1例
2018-09-28 Albertson AJ,Kummer TT 脑血管病及重症文献导读
Bow Hunter综合征也称为旋转性椎基底动脉供血不足(vertebrobasilar insufficiency),是一种罕见的疾病,特征为颈部转动时引起后循环缺血。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Bow#
73
#综合征#
90
#罕见#
71
#双侧#
85