JAMA Surg:新辅助化疗后乳腺癌患者保乳手术后乳房重建vs全乳切除对长期预后的影响
2020-10-19 MedSci原创 MedSci原创
对于乳腺癌患者,在新辅助化疗后,保乳手术后乳房重建患者的长期肿瘤学结果与全乳切除相当
乳腺癌患者在新辅助化疗(NACT)后,可选择保留乳头的乳房切除术(NSM)或保留皮肤的乳房切除(SSM)后立即进行乳房重建(IBR),近日研究人员比较了与传统的全乳切除(CM)相比,上述乳腺癌手术方案对患者长期肿瘤学结果的影响。

本次回顾性、倾向性得分匹配的病例对照研究在韩国首尔的Asan医疗中心进行。在2010年1月1日至2016年11月30日期间,共有1266名乳腺癌患者在NACT后,并进行了乳腺切除术,同时进行了或不进行乳房重建。在倾向评分匹配后,选择323例接受IBR和NSM/SSM的患者和323例单纯接受CM的患者进行长期肿瘤预后比较。研究的主要终点为5年局部无复发生存率、无病生存率、无远处转移生存率和总生存率。
IBR组的中位随访期为67个月,单纯CM组的中位随访期为68个月。IBR组患者的平均年龄为42岁,单纯CM组患者的中位年龄为46岁。IBR组和CM组在局部复发率(3.7% vs 3.4%)、区域复发率(7.1% vs 5.3%)或远处转移率(17.3% vs 18.6%)没有观察到显著差异。IBR组和CM组之间,在5年无局部复发生存率(95.6% vs 96.7%;HR:1.124),无病生存率(76.5% vs 79.9%;HR:1.089),无远处转移生存率(82.5% vs 82.5%;HR:0.941)或总生存率(92.0% vs 89.3%;HR:0.847)方面也没有显著差异。
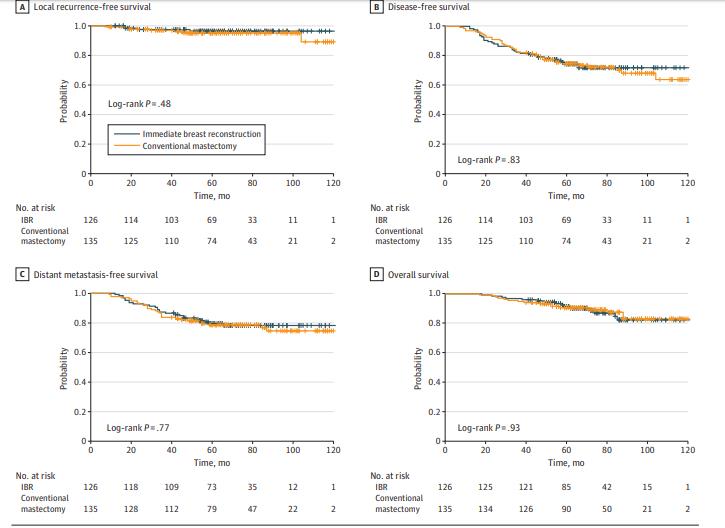
研究认为,对于乳腺癌患者,在新辅助化疗后,保乳手术后乳房重建患者的长期肿瘤学结果与全乳切除相当。
原始出处:
Zhen-Yu Wu et al. Long-term Oncologic Outcomes of Immediate Breast Reconstruction vs Conventional Mastectomy Alone for Breast Cancer in the Setting of Neoadjuvant Chemotherapy.JAMA Surg. October 14, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#全乳切除#
67
#新辅助#
83
#长期预后#
130
#乳腺癌患者#
132
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
0