NEJM、Lancet前后刊登“肉芽肿性血管炎”案例报道,还不进来学习?(敲黑板)
2016-07-05 Mechront 译 MedSci原创
案例一(Lancet):肉芽肿性血管炎并发肺动脉狭窄 患者男,23岁,急性发作性呼吸困难1天(2015年6月),不伴咳嗽、发热、感染症状、端坐呼吸、阵发性夜间呼吸困难、胸痛或心悸。 3年前患者诊断为血管炎,伴鼻窦炎肉芽肿、上肢缺血、肾损害等表现。肾活检显示局灶性坏死性肾小球肾炎;血液样本测试显示抗中性粒细胞胞浆抗体(ANCA)和抗PR3抗体。 高剂量的泼尼松龙和环磷酰胺进行初
案例一(Lancet):肉芽肿性血管炎并发肺动脉狭窄
患者男,23岁,急性发作性呼吸困难1天(2015年6月),不伴咳嗽、发热、感染症状、端坐呼吸、阵发性夜间呼吸困难、胸痛或心悸。
3年前患者诊断为血管炎,伴鼻窦炎肉芽肿、上肢缺血、肾损害等表现。肾活检显示局灶性坏死性肾小球肾炎;血液样本测试显示抗中性粒细胞胞浆抗体(ANCA)和抗PR3抗体。
高剂量的泼尼松龙和环磷酰胺进行初始治疗后,患者的疾病在临床上和免疫学上均得到缓解;此后咪唑硫嘌呤持续治疗2年。当患者急诊就诊时,每日口服强的松5 mg。
查体:窦性心动过速(105次/分)。余无异常。
辅助检查:白细胞计数升高(16 × 109/L),主要是中性粒细胞;C-反应蛋白(11 mg/L)和红细胞沉降率(38 mm/h)轻度升高。电解质、肾功能、肝功能、胸片均正常。
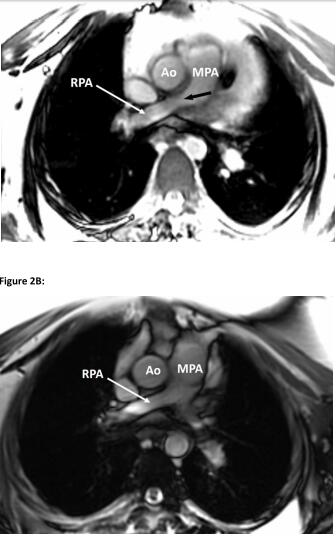
CT肺动脉造影:大量心包积液邻接严重狭窄的左肺动脉,无管腔内可见肺动脉病变或外在压缩的原因。肺实质正常。床边超声心动图:大量心包积液(最宽度达2 cm)。除了二尖瓣流入约50%的呼吸变化,没有填塞特征。肺动脉主干的峰值速度(连续波多普勒3 m/s)有流量加速。
心脏磁共振成像:明显的血管壁增厚,导致远端主肺动脉和右近端肺动脉交界处狭窄,以及更严重的左肺动脉近端狭窄。
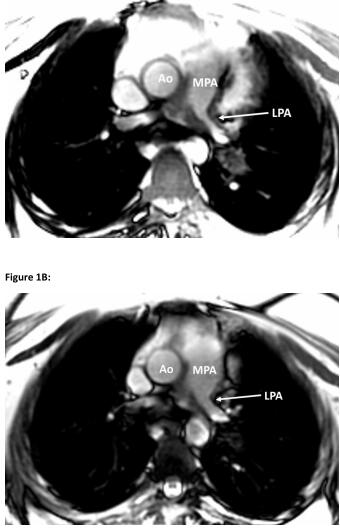
在没有动脉内阻塞和外压的情况下存在心包积液,伴心外膜突出。右和左肺动脉的血流加速,峰值速度分别为3.5米/秒和2.8米/秒。
据此患者初步诊断为:以肺动脉受损为主要表现的复发性肉芽肿性血管炎。
尿沉渣分析显示颗粒、红细胞和蛋白管型;血液测试表明ANCA阳性和抗PR3抗体阳性;证明了该诊断。颈动脉和肾动脉的双重超声没有发现额外的大血管受累的证据。
开始静脉注射甲基强的松龙和一个剂量的利妥昔单抗进行治疗。病人的呼吸困难明显改善,治疗1周后出院,每日服用强的松50 mg,1个月后重复一个剂量的利妥昔单抗。
2个月后复查心脏MRI,先前的肺动脉狭窄几乎完全缓解,在分叉处可见最小的残余血管壁增厚,以及一个小的残余心包积液。
最近的一次随访中(2015年12月),患者的强的松剂量已改为每日5 mg,他没有残留症状。
本例患者以呼吸困难为主要表现,临床上面对呼吸困难需要进行广泛的鉴别诊断,包括大气道受累、肺实质病变、肺动脉高压、心肌炎导致心力衰竭等。而本案例可以提醒大家不要忽视了呼吸困难时肺动脉狭窄的可能,尤其是CT显示肺实质正常的时候。对于这类患者,可以通过MRI进行排除诊断。
对于不明原因的近端肺动脉狭窄、壁增厚的患者因考虑到潜在的小血管炎的可能,正如本例患者。此外还应及时评估和识别多器官是否有受累,包括包括肺动脉狭窄的终末器官受累。在这种情况下的治疗,应立即启动有针对性的免疫抑制治疗。
案例二(NEJM):肉芽肿性血管炎的胃肠道并发症
患者男性,48岁,既往患有肉芽肿血管炎病史。患者因抗中性粒细胞胞浆抗体阳性,在过去的7年里一致服用硫唑嘌呤。
入院检查时发现其血肌酐水平为9.5mg/dl(840μmol/l;正常值为0.5-1.2mg/dl[ 40-110μmol/l])。尿蛋白水平为++。
入院几天后,该患者突发严重的腹痛,症状与腹膜炎一致。
CT血管造影:高度提示远端十二指肠和空肠肠壁缺血(如图A,白色箭头)与周围脂肪间隙、肠系膜水肿(黄色箭头),在腹部和盆腔存在游离液体(红色箭头)。
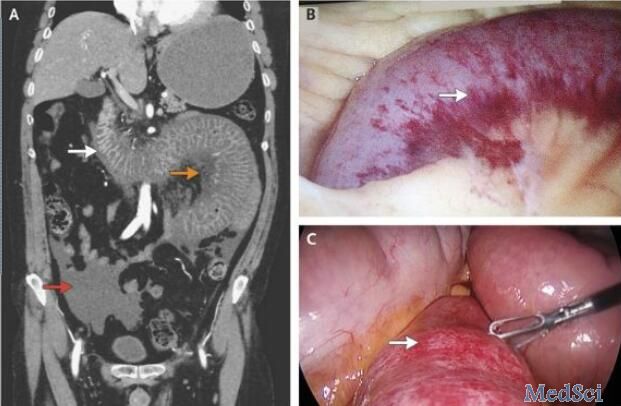
立即被送往手术室行腹腔镜下探查术,术中发现有40厘米的出血性肠段远端Treitz韧带以及腹腔积血(如图B与图C所示)。由于梗阻的出血性肠段尚有主动蠕动的功能,因此没有进行肠段切除术。术后,会诊医师认为这可能是肉芽肿血管炎导致的肠壁血管炎。
两天后,患者表现出轻微的腹部疼痛。但血肌酐水平持续升高,同时肾功能迅速恶化,进展为终末期肾衰竭,需每周行血液透析治疗三次。另外,还应用咪唑硫嘌呤药物辅助治疗,然而病情没有任何好转的迹象。
在随后的9个月的随访中,该患者表示再没有出现腹痛以及肉芽肿血管炎的相关性症状。由于其肾功能衰竭,因此他必须接受长期的血液透析治疗。
那么“肉芽肿性血管炎”是什么?
肉芽肿性血管炎(Granulomatosis with Polyangiitis, GPA),既往称为韦格纳肉芽肿(Wegener's granulomatosis, WG)。是一种坏死性肉芽肿性血管炎,属自身免疫性疾病。该病病变累及小动脉、静脉及毛细血管,偶尔累及大动脉,其病理以血管壁的炎症为特征,主要侵犯上、下呼吸道和肾脏,通常以鼻黏膜和肺组织的局灶性肉芽肿性炎症为开始,继而进展为血管的弥漫性坏死性肉芽肿性炎症。临床常表现为鼻和副鼻窦炎、肺病变和进行性肾功能衰竭。还可累及关节、眼、皮肤,亦可侵及眼、心脏、神经系统及耳等。
其临床表现因为可以累及多系统进而多种多样,
典型的GPA有三联征:上呼吸道、肺和肾病变。
一般症状有发热、疲劳、抑郁、纳差、体重下降、关节痛、盗汗、尿色改变和虚弱。其中发热最常见。大部分患者以上呼吸道病变为首发症状,如流鼻涕。肺部受累是本病基本特征之一,约50%的患者在起病时既有肺部表现,总计80%以上的患者将在整个病程中出现肺部病变。胸闷、气短、咳嗽、咯血以及胸膜炎是最常见的症状,及肺内阴影。大部分病例有肾脏病变,出现蛋白尿,红、白细胞及管型尿,严重者伴有高血压和肾病综合征,终可导致肾功能衰竭,是GPA的重要死因之一。眼受累的最高比例可至50%以上,其中约15%的患者为首发症状。GPA可累及眼的任何区域,可表现为眼球突出、视神经及眼肌损伤、结膜炎、角膜溃疡、表层巩膜炎、虹膜炎、视网膜血管炎、视力障碍等。多数患者有皮肤粘膜损伤,表现为下肢可触及的紫癜、多形红斑、斑疹、瘀点(斑)、丘疹、皮下结节、坏死性溃疡形成以及浅表皮肤糜烂等。其中皮肤紫癜最为常见。关节病变也较常见,主要有关节疼痛以及肌痛。神经系统以外周神经病变最常见,多发性单神经炎是主要的病变类型,临床表现为对称性的末梢神经病变。
关于该疾病的诊断,目前仍采用1990年美国风湿病学院分类标准:
1.鼻或口腔炎症痛性或无痛性口腔溃疡,脓性或血性鼻腔分泌物;
2.胸片异常胸片示结节、固定浸润病灶或空洞;
3.尿沉渣异常镜下血尿(RBC>5/高倍视野)或出现红细胞管型;
4.病理性肉芽肿性炎性改变动脉壁或动脉周围,或血管(动脉或微动脉)外区有中性粒细胞浸润。
符合2条或2条以上时可诊断为GPA,诊断的敏感性和特异性分别为88.2%和92.0%。
该疾病的治疗分为诱导缓解、维持缓解以及控制复发3期。治疗药物包括糖皮质激素、免疫抑制剂和其他治疗。大量证据显示,糖皮质激素加环磷酰胺联合治疗对该疾病有显著疗效。当然对于声门下狭窄、支气管狭窄等患者可以考虑外科治疗,或者如案例二的患者也需选择外科治疗。
原始出处:
Jain P, Ruchin P, Suttie J.Proximal pulmonary artery stenosis: a rare manifestation of granulomatosis with polyangiitis.Lancet. 2016 Jun 4;387(10035):2349-50. doi: 10.1016/S0140-6736(16)00584-5.
Hamzeh M. Halawani, M.D., and Mohamed Khalife, M.D. Gastrointestinal Complication of Granulomatosis with Polyangiitis N Engl J Med 2016; 374:2159June 2, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Lancet#
45
#肉芽肿性血管炎#
50
谢谢分享学习
89
好文章,受益
89
不错哦继续关注
97
好文章,赞一个!深入学习,探究。
102
好文,值得学习,赞一个。
91
#血管炎#
55
#肉芽肿#
53
少见,学习了
84