J Cancer:苏州大学教授构建出可准确预测白血病的网络生物标志物
2017-03-02 MedSci MedSci原创
网络生物标志物相比于单个标志物可以更加有效的区分白血病的疾病样本和正常样本。网络生物标志物提供了诊断白血病的有效方法,也有助于进一步了解白血病的分子基础。
白血病是发达国家癌症死亡的主要原因。国内外一直努力寻找用于白血病诊断的分子生物标志物,但由于白血病的异质性和复杂性,它的发生发展涉及多个分子组分之间的相互作用。因此,目前普遍使用的单个分子标志物具有一定的局限性。网络生物标志物被认为在疾病表征中优于个体分子。
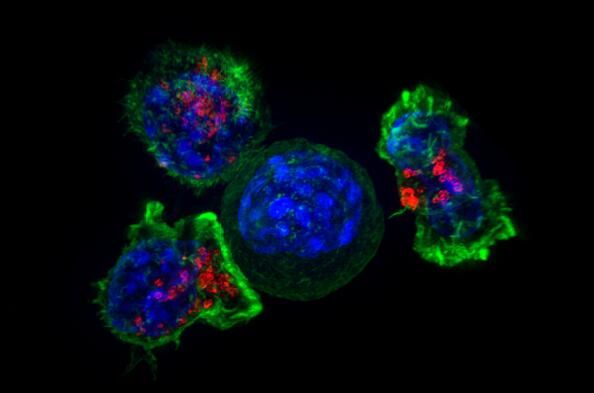
该研究整合蛋白质相互作用网络和基因表达数据,在系统层面上对白血病的关键基因进行模块化分析,构建可以为诊断白血病提供依据的网络生物标志物。首先,我们选择蛋白质相互作用网络数据库 PINA 和数据库 GeneGo中白血病相关基因,重建白血病特异性蛋白质相互作用网络。接下来,进一步整合基因表达数据 以识别具有白血病相关性的活性模块。最后,评估候选网络生物标志物的诊断性能。最终得到一个包含97个基因和400条映射关系的网络用于准确诊断白血病。功能富集分析结果显示,该网络标志物中的基因主要富集在白血病等癌症相关通路上。
网络生物标志物相比于单个标志物可以更加有效的区分白血病的疾病样本和正常样本。网络生物标志物提供了诊断白血病的有效方法,也有助于进一步了解白血病的分子基础。
原始出处:Xuye Yuan, Jiajia Chen, Yuxin Lin,et al.Network Biomarkers Constructed from Gene Expression and Protein-Protein Interaction Data for Accurate Prediction of Leukemia.J Cancer 2017; 8(2):278-286. doi:10.7150/jca.17302
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#标志物#
0
#苏州大学#
70
#生物标志#
69
#生物标志#
75
早诊断,早治疗
114