盘点:关于甲氨蝶呤用药新近进展
2016-08-30 MedSci MedSci原创
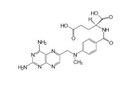
甲氨蝶呤为抗叶酸类抗肿瘤药,主要通过对二氢叶酸还原酶的抑制而达到阻碍肿瘤细胞的合成,而抑制肿瘤细胞的生长与繁殖。在用甲氨蝶呤后,加用甲酰四氢叶酸钙,可直接向细胞提供四氢叶酸辅酶,避开甲氨蝶呤的抑制作用,以减轻其细胞毒的毒性作用。甲氨蝶呤(MTX),是一种既有抗炎又有抗肿瘤特性的有效叶酸拮抗剂,广泛应用于很多自身免疫性疾病,包括类风湿性关节炎(RA),银屑病,和炎症性肠病(IBD)的治疗。在过去
本文系梅斯医学(MedSci)原创编译整理,转载需授权!更多资讯,请下载"辣眼睛的医学科研神器之梅斯医学APP”!扫一下二维码即可: 

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了,赞一个!!!
100
学习了,赞一个!!!
0
学习了,赞一个!!!
108
学习了,赞一个!!!
100
学习了,赞一个!!!
99
学习学习好好学习
59
这个很好用
65