汇总!近期抑郁症相关研究进展
2017-02-21 MedSci MedSci原创
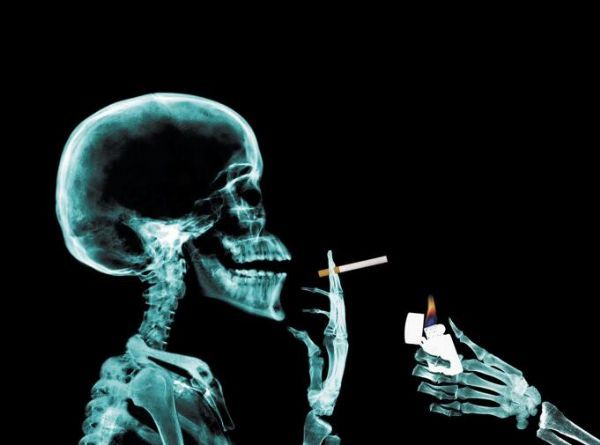
抑郁症又称抑郁障碍,以显著而持久的心境低落为主要临床特征,是心境障碍的主要类型。临床可见心境低落与其处境不相称,情绪的消沉可以从闷闷不乐到悲痛欲绝,自卑抑郁,甚至悲观厌世,可有自杀企图或行为;甚至发生木僵;部分病例有明显的焦虑和运动性激越;严重者可出现幻觉、妄想等精神病性症状。每次发作持续至少2周以上、长者甚或数年,多数病例有反复发作的倾向,每次发作大多数可以缓解,部分可有残留症状或转为慢性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关研究#
67
谢谢分享,学习了!
109
#研究进展#
64
望科学家能早日攻克抑郁症,造福人类
82
很好的内容
85
抑郁症是顽疾,希望可以根除
74
抑郁症可见心境低落与其处境不相称。
58
学习了许多先进的医学知识
60
长达数年之久
52
归纳的真好!
67