巨型基底动脉动脉瘤表现为第三脑室占位一例
2019-06-24 龚敏 王淼 游潮 华西医学
患者,女,48岁。因“头痛伴下肢乏力2个月”于2017年8月28日入院。2个月前患者无明显诱因出现头痛,间断发作,伴下肢无力,行走时摔倒,无头晕、恶心、呕吐、意识障碍、无大小便失禁等症状。到当地医院就诊,头部CT提示:第三脑室占位病变。
1.病例介绍
患者,女,48岁。因“头痛伴下肢乏力2个月”于2017年8月28日入院。2个月前患者无明显诱因出现头痛,间断发作,伴下肢无力,行走时摔倒,无头晕、恶心、呕吐、意识障碍、无大小便失禁等症状。到当地医院就诊,头部CT提示:第三脑室占位病变。
既往史:20年前行剖宫产手术,2年前行腹腔镜胆囊切除术。体格检查:患者神清语利,双侧瞳孔等大等圆,对光反射灵敏,高级神经活动正常,四肢肌力、肌张力正常,生理反射存在,病理反射未引出。入院后完善血常规、肝肾功能、电解质、凝血全套、输血全套、人绒毛膜促性腺激素等未见明显异常,心电图及胸部X线平片未见明显异常。
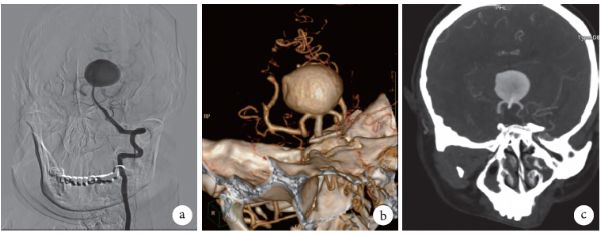
头部CT显示第三脑室占位,无蛛网膜下腔出血(图1a)。完善头部MRI检查提示:第三脑室占位,伴有不均匀强化(图1b~1d)。后进一步完善头部CT血管造影(CT angiography,CTA)及行全脑数字减影血管造影(digital subtraction angiography,DSA)等提示:第三脑室内有一29mm×27mm×25mm的基底动脉动脉瘤(图2)。经全科讨论,建议采取介入栓塞治疗,但患者家属拒绝进一步治疗,于2017年9月5日出院。
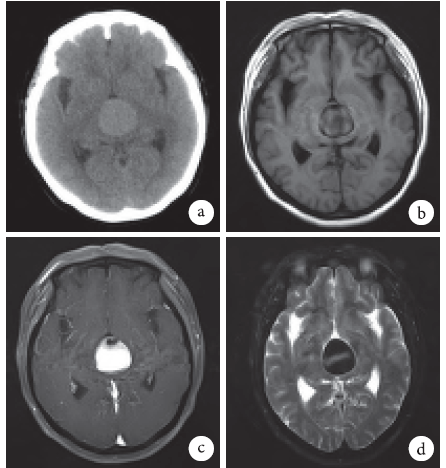
图1 患者CT和MRI扫描像a.CT扫描,显示第三脑室内有1个圆形肿块病变,呈高密度影;b~d.MRI扫描,显示第三脑室内占位病变,伴有不均匀强化;b.T1加权像;c.T1加权像增强;d.T2加权像
图2 患者头部相关检查像可见基底动脉巨型动脉瘤,大小约29mm×27mm×25mm;a.DSA;b.3D-CT;c.CTA
2.讨论
颅内巨型动脉瘤为直径>2.5 cm的动脉瘤,发病率约占所有动脉瘤的5%。位于第三脑室内的巨型动脉瘤很罕见,经常被认为是第三脑室占位病变,导致误诊。从CT特点来判断病变是否为动脉瘤或肿瘤是很困难的。血管造影被认为是诊断动脉瘤的金标准。这种疾病最常见的临床表现为脑积水。脑室腹腔分流术(ventculoperitioneal shunt,VP)及第三脑室底造瘘(endoscopic third ventriculostomy,ETV)可供选择来缓解脑积水。
①临床特点。据报道,在不同的研究中,表现为占位病变的动脉瘤的发生率为23%~64%。巨型动脉瘤表现为第三脑室病变更少。我们回顾25例表现为第三脑室占位病变的动脉瘤病例,其中男11例,女14例;年龄32~82岁,平均(62.6±11.4)岁。其中第25例即为本文报道患者。大部分动脉瘤位于基底动脉(20例),2例位于后交通动脉,2例位于前交通动脉,1例位于大脑中脑动脉。第三脑室内动脉瘤最常见的临床症状为脑积水(21/25),有时伴有脑出血、蛛网膜下腔出血(subarachnoid hemorrhage,SAH)和癫痫发作等。共有16个巨型动脉瘤,7个大型动脉瘤,1个大脑中动脉小型动脉瘤,1个基底动脉一般型动脉瘤。25例患者中,21例动脉瘤内有部分血栓形成,1例完全血栓形成和3例无血栓形成。8例患者动脉瘤发生破裂,包括4个巨型、2个大型、1个一般型和1个微小型动脉瘤。
②神经影像学。大多数患者在有临床症状后接受了CT或MRI检查。从CT扫描的特点来判断病变是否为动脉瘤或肿瘤是困难的。但病变大小和脑积水能通过CT体现。MRI在鉴别肿瘤和动脉瘤方面起着重要的作用,它可确定是否有瘤内血栓形成、病变的具体位置、血流动力学以及病变与载瘤血管的关系。血管成像是区分血管病变和占位病变的重要检查。包括CTA、磁共振血管造影和DSA。DSA是诊断动脉瘤的金标准,它能准确地了解动脉瘤的位置,并显示其与载瘤血管和邻近动脉的关系,并可靠地描述动脉瘤腔内的情况。然而,血管造影的诊断率并不能达到100%。Liu等报道了1例第三脑室内基底动脉瘤伴有完全血栓形成的病例,CT和MRI并未发现动脉瘤;为明确诊断和治疗,他们手术切除了第三脑室病变,术后发现病变为血栓,最终诊断为动脉瘤。但对于非完全血栓性动脉瘤患者,血管造影在诊断中起着重要的作用。
③治疗及预后。在文献回顾中,21例患者有脑积水,11例行VP分流术,2例行ETV,8例接受VP分流的患者预后良好,1例接受ETV的患者也有良好的预后。然而,在未处理动脉瘤前行VP分流术有可能会导致动脉瘤持续增大或破裂。但文献中提到的接受了VP或ETV的患者均未出现动脉瘤破裂,仅有3例患者发生术前动脉瘤破裂。术前有SAH或脑内血肿被认为是行ETV的一个危险因素。有研究认为,对于术前发生动脉瘤破裂的患者不应行ETV手术,而推荐行VP分流术来改善脑积水。
在未破裂的动脉瘤中,VP或ETV都可以选择。颅内巨型动脉瘤很少发生破裂,而肿块效应或缺血的症状是患者的主要风险。回顾的25例患者中,只有8例通过夹闭或介入治疗动脉瘤,5例受益于手术,3例死亡;17例未接受动脉瘤的治疗;另有16例有巨大动脉瘤,但只有3例接受手术治疗。同时,18例取得了良好的预后,7例死亡。这类患者脑积水的发病率很高,且多数是因脑积水而就诊。因此脑积水的治疗是患者就诊的主要目的。而对于动脉瘤的处理,大多数采取保守治疗,尤其是巨型动脉瘤。巨型动脉瘤表现为第三脑室占位很罕见。在治疗前应行脑血管造影以明确诊断。第三脑室内巨型动脉瘤最常见的临床表现是脑积水,VP或ETV可以改善其症状,而对于动脉瘤,保守治疗是一个很好的选择。
原始出处:
龚敏,王淼,游潮.巨型基底动脉动脉瘤表现为第三脑室占位一例[J].华西医学,2018,33(06):774-776.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#脑室占位#
76
谢谢了,学习
101
#基底动脉#
76
#脑室#
71
666
101