Endeavor R与Cypher R支架对直接PCI的STEMI患者安全有效
2012-05-06 王嘉玲 医学论坛网
最近,北京朝阳医院的王乐丰在第10届中国介入心脏病学(CIT)大会最新临床试验与特色研究专场上公布的一项研究显示:Endeavor R西罗莫司与Cypher R佐他莫司洗脱支架对于直接经皮冠脉介入(PCI)治疗的ST段抬高型心肌梗死(STEMI)患者是安全有效的;随访12个月时,置入EndeavorR西罗莫司洗脱支架的再狭窄率及靶病变血运重建(TLR)率高于CypherR佐他莫司洗脱支架。
最近,北京朝阳医院的王乐丰在第10届中国介入心脏病学(CIT)大会最新临床试验与特色研究专场上公布的一项研究显示:Endeavor R西罗莫司与Cypher R佐他莫司洗脱支架对于直接经皮冠脉介入(PCI)治疗的ST段抬高型心肌梗死(STEMI)患者是安全有效的;随访12个月时,置入EndeavorR西罗莫司洗脱支架的再狭窄率及靶病变血运重建(TLR)率高于CypherR佐他莫司洗脱支架。
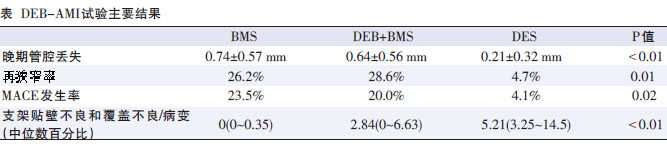
既往几项已发表的研究显示,药物洗脱支架(DES)用于直接PCI的STEMI患者安全有效,能降低再狭窄及主要心脏不良事件(MACE)的发生率。但这些研究没有针对性地评估Cypher R与Endeavor R之间的临床及血管造影终点。
在此研究中,随访至1年时的患者达843例(97.8%)。6个月时 ,EndeavorR和CypherR的复合MACE分别为4.5%和3.5%(P=0.48),靶病变血运重建(TLR)率分别为1.3%和0.7%(P=0.35),支架再狭窄率分别为1.1%和0.2%(P=0.09),心梗发生率分别为0.4%和0.7%(P=0.61)。12个月时,Endeavor R和Cypher R的心源性死亡发生率分别为2.9%和2.1%(P=0.38),TLR发生率分别为2.1%和0.6%(P=0.05),支架再狭窄率分别为2.2%和0.2%(P=0.01),支架内血栓形成率分别为1.5%和1.3%(P=0.75),心梗发生率分别为1.3%和1.1%(P=0.78),卒中发生率分别为0.6% 和0.4%(P=0.68),出血发生率分别为1.7%和1.3%(P=0.24)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cypher#
62
#Endeavor#
50
#患者安全#
56
#STEMI患者#
69
#直接PCI#
62
#STEM#
71