常见消化道瘘的影像学表现--胆囊内瘘
2015-02-03 首都医科大学附属北京朝阳医院 蒋涛 中国医学论坛报
胆囊内瘘多是由胆囊结石引起的自发性瘘,患者几乎都有急慢性胆囊炎发作史。病程中胆囊与邻近脏器尤其是胆总管、十二指肠发生炎症粘连,当结石嵌顿于胆囊颈部、胆囊内胆汁引流不畅、压力升高,胆囊壁血供受限,最终导致胆囊壁发生坏疽、穿透邻近脏器的壁形成内瘘及胆囊内容物包括结石排入肠道内。 胆囊内瘘的多层螺旋CT表现主要包括以下4点:①急慢性胆囊炎,既往胆囊结石病史,再次扫描胆囊内结石消失,相应十二指肠
胆囊内瘘多是由胆囊结石引起的自发性瘘,患者几乎都有急慢性胆囊炎发作史。病程中胆囊与邻近脏器尤其是胆总管、十二指肠发生炎症粘连,当结石嵌顿于胆囊颈部、胆囊内胆汁引流不畅、压力升高,胆囊壁血供受限,最终导致胆囊壁发生坏疽、穿透邻近脏器的壁形成内瘘及胆囊内容物包括结石排入肠道内。
胆囊内瘘的多层螺旋CT表现主要包括以下4点:①急慢性胆囊炎,既往胆囊结石病史,再次扫描胆囊内结石消失,相应十二指肠部位或胃腔、结肠内发现高密度结石影;②胆囊周围出现炎性包块影;③胆囊内或胆管内积气;④部分患者可出现结石性肠梗阻,其中第3条为较特异性的影像学表现。

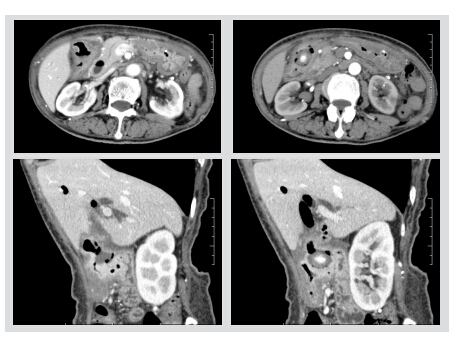
图 女性,66岁,既往慢性胆囊炎,胆囊结石病史。CT增强扫描及斜位重建显示胆囊壁及结肠壁明显增厚,连续性中断,结肠内可见高密度结石影,胆囊内及肝内胆管、胆总管积气。术后病理证实为胆囊内瘘
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







比较少见的
182
非常好的文章,学习
107
?学习了
113
#消化道#
80