PNAS:消化道细菌A. muciniphila或可用于预防肥胖
2013-05-15 PNAS 生物360
日前,比利时与荷兰的研究发现,消化道细菌Akkermansia muciniphila可能在维持消化道粘膜屏障和防止肥胖相关代谢疾病方面起到了一个关键的作用。研究人员发现,生活在消化道的营养丰富的粘液层的主要的细菌A. muciniphila的丰富程度在肥胖和II型糖尿病小鼠体内减少了。研究人员还观察到了,让这些小鼠服用低聚果糖益生元(oligofructose prebiotics)能恢复A.
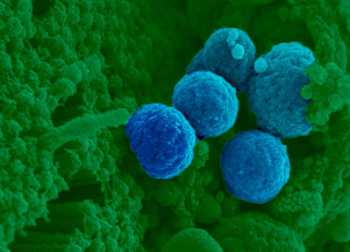
日前,比利时与荷兰的研究发现,消化道细菌Akkermansia muciniphila可能在维持消化道粘膜屏障和防止肥胖相关代谢疾病方面起到了一个关键的作用。
研究人员发现,生活在消化道的营养丰富的粘液层的主要的细菌A. muciniphila的丰富程度在肥胖和II型糖尿病小鼠体内减少了。研究人员还观察到了,让这些小鼠服用低聚果糖益生元(oligofructose prebiotics)能恢复A. muciniphila的丰富程度,这与消化道屏障的改善以及肥胖相关代谢疾病的逆转相关,这些代谢疾病包括脂肪重量增加、脂肪组织炎症以及胰岛素耐受。提供A. muciniphila增加了控制葡萄糖和肠道平衡的内源性大麻素的肠道水平,并且阻碍了饮食诱导的粘膜屏障厚度的减少。
研究人员发现,这些效应需要活的A. muciniphila作为疗法,而热灭活的A. muciniphila不会改善这种代谢情况或者小鼠的粘液层厚度。这些结果表明A. muciniphila可能在消化道屏障功能、代谢炎症和脂肪储存方面起到了一个关键的作用,而且研究人员提出,可以将A. muciniphila用于开发预防肥胖及其相关代谢疾病的疗法。
与肥胖相关的拓展阅读:
- PLoSOne:我国肥胖人群缺血性卒中风险增加
- [PUDF2013]邹大进:肥胖糖尿病患者的血脂管理策略
- [PUDF2013]李光伟:胰岛素抵抗和肥胖,鸡生蛋还是蛋生鸡?
- [PUDF2013]肥胖和营养在青年人1型和2型糖尿病中的作用
- [PUDF2013]宁光:让肥胖对糖尿病有利
- [PUDF2013]周翔海:中国肥胖合并2型糖尿病患者的特征 更多信息请点击:有关肥胖更多资讯

Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity
Abstract
Obesity and type 2 diabetes are characterized by altered gut microbiota, inflammation, and gut barrier disruption. Microbial composition and the mechanisms of interaction with the host that affect gut barrier function during obesity and type 2 diabetes have not been elucidated. We recently isolated Akkermansia muciniphila, which is a mucin-degrading bacterium that resides in the mucus layer. The presence of this bacterium inversely correlates with body weight in rodents and humans. However, the precise physiological roles played by this bacterium during obesity and metabolic disorders are unknown. This study demonstrated that the abundance of A. muciniphila decreased in obese and type 2 diabetic mice. We also observed that prebiotic feeding normalized A. muciniphila abundance, which correlated with an improved metabolic profile. In addition, we demonstrated that A. muciniphila treatment reversed high-fat diet-induced metabolic disorders, including fat-mass gain, metabolic endotoxemia, adipose tissue inflammation, and insulin resistance. A. muciniphila administration increased the intestinal levels of endocannabinoids that control inflammation, the gut barrier, and gut peptide secretion. Finally, we demonstrated that all these effects required viable A. muciniphila because treatment with heat-killed cells did not improve the metabolic profile or the mucus layer thickness. In summary, this study provides substantial insight into the intricate mechanisms of bacterial (i.e., A. muciniphila) regulation of the cross-talk between the host and gut microbiota. These results also provide a rationale for the development of a treatment that uses this human mucus colonizer for the prevention or treatment of obesity and its associated metabolic disorders.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CIN#
50
#PNAS#
71
#消化道#
64
我觉的这是正确的
104