令人担忧!Delta变异毒株更具传染性,将席卷全球?
2021-06-17 JACKZHAO MedSci原创
世卫组织称目前在74个国家和地区Delta变异毒株被发现,并继续迅速传播,人们担心它可能会成为全球的主流毒株。

新冠疫情爆发一年多以来,已经有多种变异毒株引起过特别的关注。最引人关注的毒株包括最先出现在英国肯特的Alpha、南非的Beta、巴西的Gamma,和印度的Delta。
其中来自印度的Delta变异毒株最为活跃,已在全球持续传播,世卫组织称目前在74个国家和地区Delta变异毒株被发现,并继续迅速传播,人们担心它可能会成为全球的主流毒株。
6月14日,《柳叶刀》在线发表通讯文章指出,来自印度变种B 1.617.2迅速成为苏格兰地区SARS-CoV-2 的优势毒株。 而Alpha VOC(以前称为 Kent VOC、B.1.1.7 或 S 基因阴性)是以前优势毒株,但它已迅速被取代。
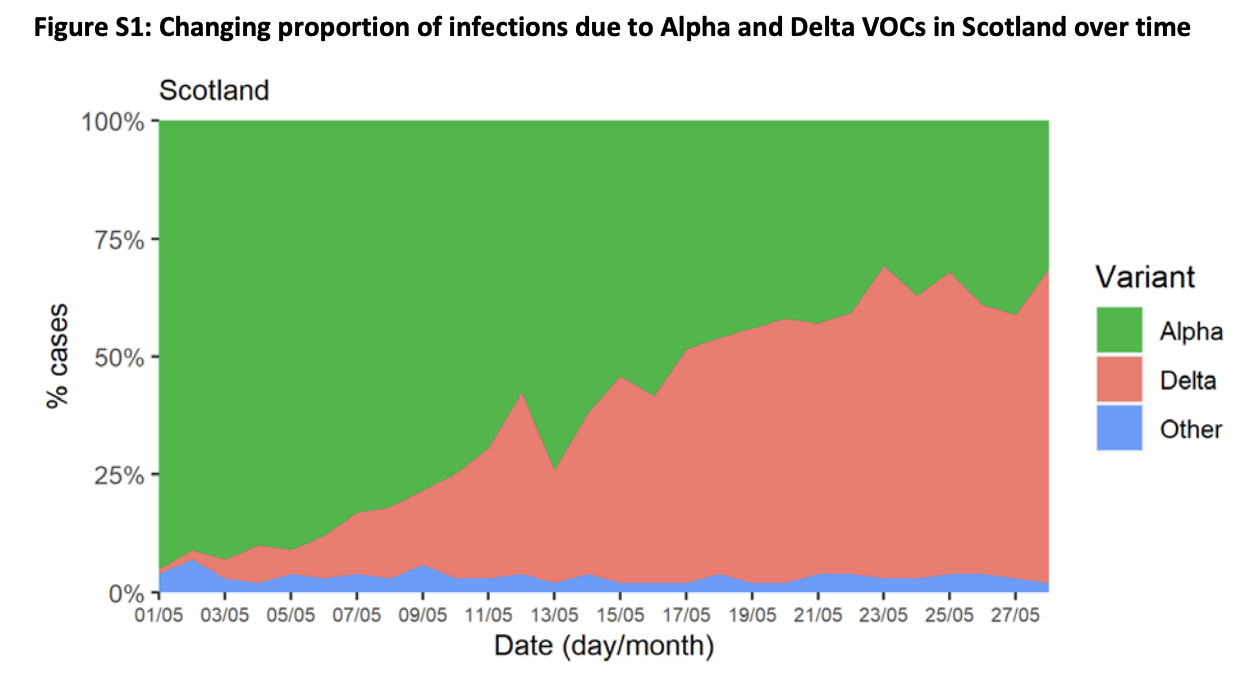
苏格兰公共卫生机构研究苏格兰地区的COVID-19 监测平台EAVE II从 2021 年 4 月 1 日到 2021 年 5 月 28 日的测序数据进行队列分析发现,97% 的 S 基因在苏格兰测序的阳性病例是 Delta 变体,并且 99% 的 Delta 变体是 S 基因阳性。与 alpha (B.1.1.7) 变体相比,住院人数翻了一番。
前美国FDA局长斯科特·戈特利布周日表示,一种被称为 Delta 变体的冠状病毒株很可能成为美国新感染的主要来源,并可能在秋季导致新的疫情爆发, 未接种疫苗的美国人最危险。“目前,在美国,感染率约为 10%。每两周增加一倍,”戈特利布在“面对国家”节目中说。 “这并不意味着我们会看到感染率急剧上升,但这确实意味着这将接管。而且我认为风险真的在于秋季,这可能会引发新的流行病 秋天。”
mRNA疫苗似乎能有效控制Delta变体,这突显了公共疫苗接种运动的重要性。“mRNA 疫苗似乎非常有效,两剂针对这种变体的疫苗。强生和阿斯利康的病毒载体疫苗似乎也有效,大约有 60% 有效率。mRNA 疫苗大约有 88% 有效率,在疫苗接种率低的地区,新爆发的风险最为明显。
伦敦帝国理工学院的尼尔弗格森(Ferguson)称,Delta 对 Alpha 的传染优势的估计已经缩小, 60% 可能是最好的估计。模型表明,任何第三波感染都可能与英国冬季的第二波感染相当(这是由在英格兰东南部肯特首次发现的 Alpha 变种推动的)。

但目前尚不清楚住院人数激增将如何转化为死亡人数的增加,因为需要更多细节来了解疫苗在多大程度上预防Delta变异毒株严重疾病。他说:“我们很有可能会看到至少在住院人数方面具有可比性的第三波。”“我认为死亡人数可能会更低,疫苗具有很强的保护作用......仍然可能非常令人担忧。但存在很多不确定性。”
尼尔弗格森表示,Delta 变种相对于 Alpha 的多达四分之一的传播优势可能来自其对疫苗的免疫逃逸,并称这是对其优势的“贡献,但不是压倒性的贡献”。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#传染性#
84
学习了
80
#变异#
44
学习了
85
学习了
83
…
104