Lancet:血管内弹簧圈比外科夹闭治疗破裂动脉瘤死亡风险显著下降(ISAT试验18年随访结果)
2015-05-11 MedSci MedSci原创
ISAT研究1年随访发现,动脉瘤弹簧圈比夹闭能够降低死亡和依赖的比例,但是中期随访发现弹簧圈组患者目标动脉瘤需要再次治疗的人数增加。2015年2月Lancet上发表了ISAT长期(18年)随访结果。 Kaplan-Meier plot of cumulative risk of rebleeding from target (treated) aneurysm later
ISAT研究1年随访发现,动脉瘤弹簧圈比夹闭能够降低死亡和依赖的比例,但是中期随访发现弹簧圈组患者目标动脉瘤需要再次治疗的人数增加。2015年2月Lancet上发表了ISAT长期(18年)随访结果。
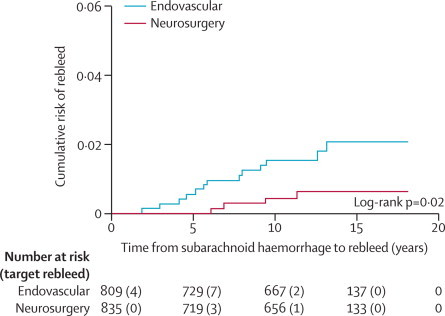
Kaplan-Meier plot of cumulative risk of rebleeding from target (treated) aneurysm later than 1 year after subarachnoid haemorrhage
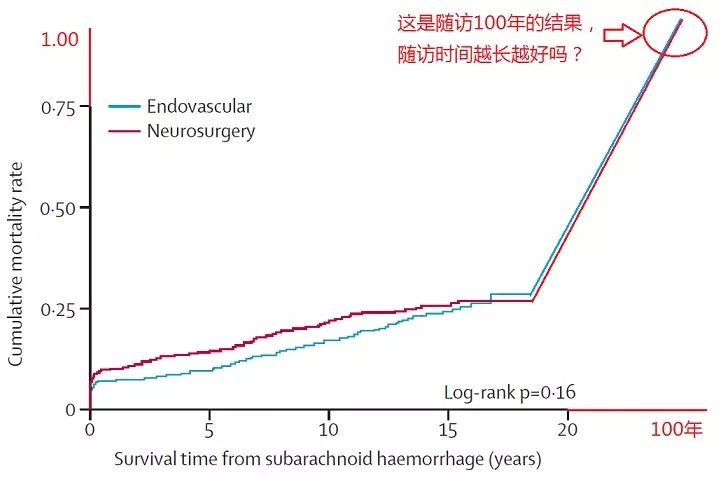
在10年时,血管内弹簧圈和外科夹闭组生存的比例分别为83%和79%(OR=1.35,95%CI,1.06-1.73)。10年收到的问卷调查显示两组mRS评分0-2分的比例分别为82%和78%(OR=1.25;95%CI,0.92-1.71)。10年时血管内弹簧圈组患者生存和mRS评分0-2分的比例更多(OR=1.34;95%CI,1.07-1.67)。
标化后死亡率
| Deaths | Expected deaths | Standardised mortality ratio (95% CI) | |
|---|---|---|---|
| All patients | 246 | 175 | 1·40 (1·23–1·58) |
| Women | 146 | 106 | 1·37 (1·15–1·59) |
| Men | 100 | 69 | 1·45 (1·17–1·73) |
| Endovascular group | 122 | 89 | 1·37 (1·13–1·62) |
| Neurosurgery group | 124 | 87 | 1·43 (1·18–1·67) |
最后作者认为,虽然两组间依赖的比率增加没有差异,但是外科手术夹闭动脉瘤组死亡或依赖的比例更高。血管内弹簧圈比外科夹闭再出血的风险更高,但是这种风险较小,10年时血管内弹簧圈组无残疾生存的可能性更高。
原始出处:
Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS.The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the International Subarachnoid Aneurysm Trial (ISAT).Lancet. 2015 Feb 21;385(9969):691-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
72
#随访结果#
72
想想以前的手术
142
进步了
154
有偏移存在吧'
147
看看
162
#死亡风险#
54
有价值
57