JAMA:复方新诺明对中重度特发性肺纤维化患者死亡,肺移植或住院的影响
2020-12-30 MedSci原创 MedSci原创
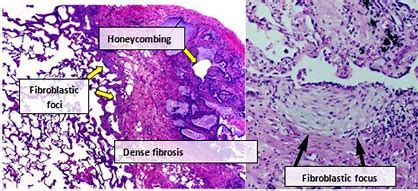
特发性肺纤维化(IPF)是一种慢性、进行性、纤维化性间质性肺疾病,病变局限在肺脏,好发于中老年人群,其肺组织学和/或胸部高分辨率CT(HRCT)特征性表现为普通型间质性肺炎(UIP),病因不清。按病程
特发性肺纤维化(IPF)是一种慢性、进行性、纤维化性间质性肺疾病,病变局限在肺脏,好发于中老年人群,其肺组织学和/或胸部高分辨率CT(HRCT)特征性表现为普通型间质性肺炎(UIP),病因不清。按病程有急性、亚急性和慢性之分,本病多为散发,据统计,每年整体人群中的患病率约(2~29)/10万,且呈逐渐增长趋势,估计以每年11%的比例增长。在美国特发性肺纤维化患者大约有100000人,欧盟地区大约有110000人,而且每年欧盟地区新增IPF患者35000人。日本每年整体人群中的IPF患病率约(2.23~10)/10万,实际值远高于这个数目。我国作为一个老龄化严重的国家,目前IPF患病人数也是逐年增加,保守估计至少在50万左右。作为一种慢性间质性肺病,IPF起病隐匿、病情逐渐加重,也可表现为急性加重。IPF诊断后的平均生存期仅2.8年,死亡率高于大多数肿瘤,IPF被称为一种“类肿瘤疾病”。
特发性肺纤维化(IPF)的预后较差,治疗选择有限。IPF患者的肺微生物群已改变,肺内细菌负担与死亡率有关;2013年一项小型随机对照研究表明,使用复方新诺明(trimethoprim-sulfamethoxazole)对IPF有益处,能极其显著改善FVC,6MWT,以及患者的生存,尤其是减少79%的死亡风险。但是,研究一经发表,也备受质疑。因此,2018年左右开始了本项研究。研究注册于ISRCTN Identifier: ISRCTN17464641
事实上,复方新诺明,也叫复方磺胺甲基异恶唑,是一款古老的药物,为磺胺类抗菌药,是磺胺甲恶唑(SMZ)与甲氧苄啶(TMP)的复方制剂,对非产酶金黄色葡萄球菌、化脓性链球菌、肺炎链球菌、大肠埃希菌、克雷伯菌属、沙门菌属、变形杆菌属、摩根菌属、志贺菌属等肠杆菌科细菌、淋球菌、脑膜炎奈瑟菌、流感嗜血杆菌均具有良好抗菌作用。但是,整体疗效一般,因此,近年来在临床应用日渐减少。
本项研究在英国39个专科间质性肺病中心进行的342例IPF,呼吸困难(医学研究委员会呼吸困难评分≥1)和肺功能受损(预计肺活量为75%)的患者的双盲,安慰剂对照,平行随机试验 在2015年4月(首次患者就诊)和2019年4月(最后一次患者随访)之间。
研究参与者被随机分为12个月至42个月,每天两次接受960 mg口服复方新诺明(n = 170)或匹配的安慰剂(n = 172)。所有患者每天口服一次5 mg叶酸。
主要终点为是全因死亡,肺移植或首次急诊入院。有15个次要结局,包括主要终点呼吸相关事件的各个组成部分,肺功能(强制肺活量和气体转移)和患者报告的结局(医学研究委员会呼吸困难量表,EuroQol 5D问卷,咳嗽严重程度,莱赛斯特咳嗽生命质量问卷(LCQ)和King's Brief Interstitial Lung Disease问卷得分)。
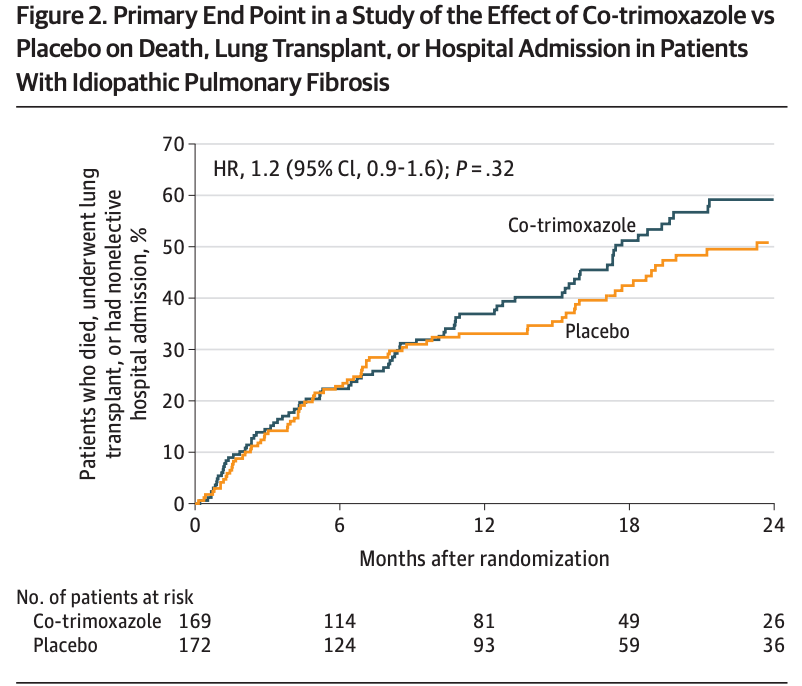
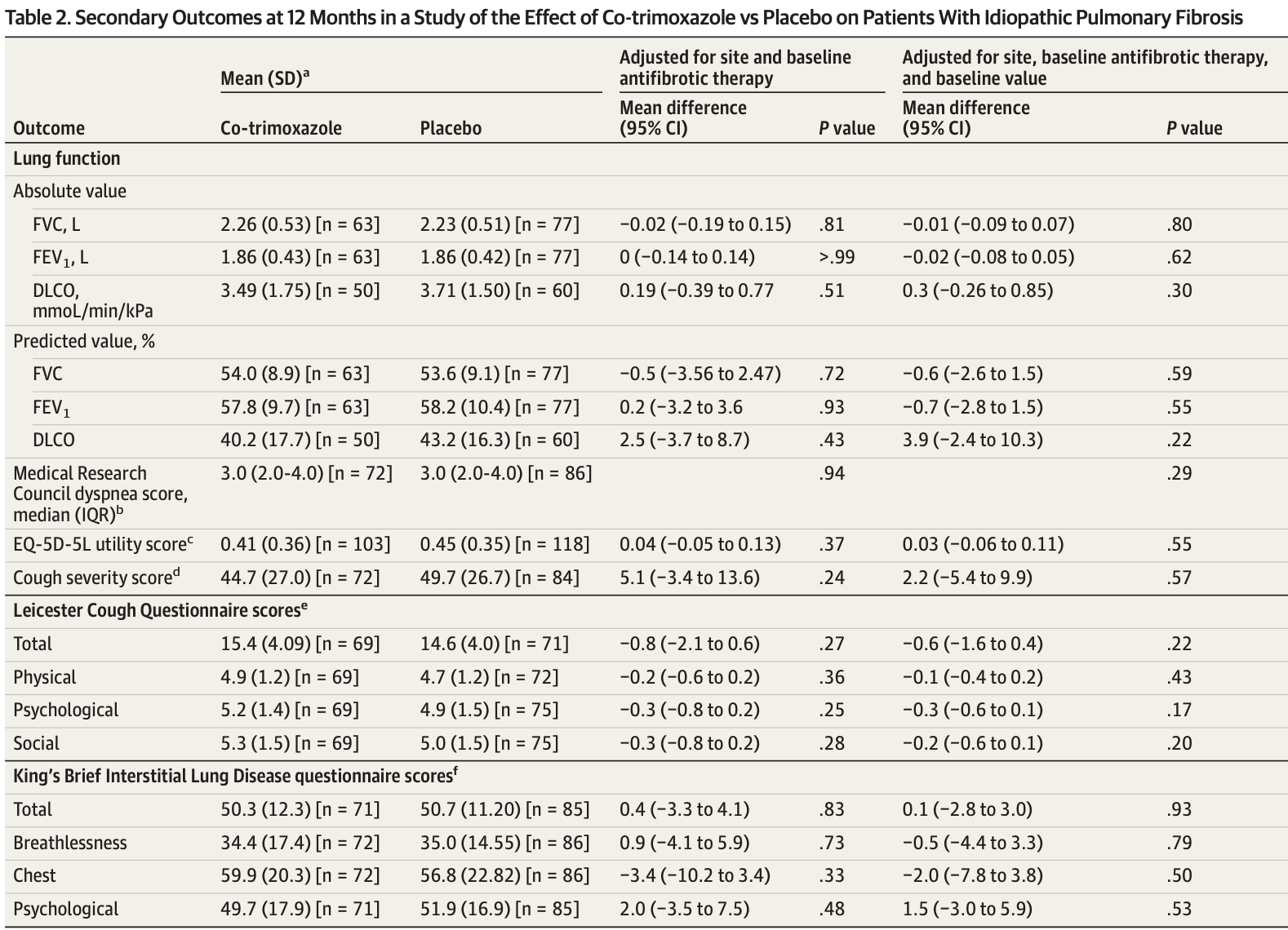
共342名随机分组的人(平均年龄71.3岁)中,有283名(83%)完成了试验。随访的中位时间(四分位间距)为1.02(0.35-1.73)年。随机分配给复方新诺明和安慰剂组的参与者每人年随访的事件分别为0.45(84/186)和0.38(80/209),危险比为1.2([95%CI,0.9 -1.6];P = 0.32)。其他事件结局,肺功能或患者报告的结局在统计学上无显着差异。复方新诺明组的患者有696例不良反应(恶心[n = 89],腹泻[n = 52],呕吐[n = 28]和皮疹[n = 31]),安慰剂组的患者有640例不良反应事件(恶心[n = 67],腹泻[n = 84],呕吐[n = 20]和皮疹[n = 20])。
结果显示,在中度或重度IPF患者中,与安慰剂相比,口服复方新诺明口服治疗并没有减少全因死亡,移植或急诊住院的复合终点。
事实上,在今年另外有一项复方新诺明用于IPF的真实世界研究也正在开展,叫CleanUP-IPF。但是,这项研究认为复方新诺明对中重度的IPF并未观察到获益,对后续的研究也可能带来一定的影响。
在线使用:莱赛斯特咳嗽生命质量问卷(LCQ)
原始出处:
Treating idiopathic pulmonary fibrosis with the addition of co-trimoxazole: a randomised controlled trial.Thorax. 2013 Feb;68(2):155-62.
Wilson AM, Clark AB, Cahn T, Chilvers ER, Fraser W, Hammond M, Livermore DM, Maher TM, Parfrey H, Swart AM, Stirling S, Thickett DR, Whyte M; EME-TIPAC team. Effect of Co-trimoxazole (Trimethoprim-Sulfamethoxazole) vs Placebo on Death, Lung Transplant, or Hospital Admission in Patients With Moderate and Severe Idiopathic Pulmonary Fibrosis: The EME-TIPAC Randomized Clinical Trial.JAMA. 2020 Dec 8;324(22):2282-2291. doi: 10.1001/jama.2020.22960.
Design and rationale of a multi-center, pragmatic, open-label randomized trial of antimicrobial therapy - the study of clinical efficacy of antimicrobial therapy strategy using pragmatic design in Idiopathic Pulmonary Fibrosis (CleanUP-IPF) clinical trial.Respir Res. 2020 Mar 12;21(1):68. doi: 10.1186/s12931-020-1326-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#特发性#
44
#患者死亡#
59
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
70
#特发性肺纤维化##老药新用#
231
好文章!
95
学习了
108