JAHA:房颤发病率、患病率和死亡率的时间变化趋势!
2017-04-29 xing.T MedSci原创
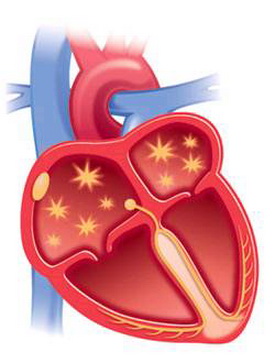
在大型的一般实践人群中,房颤发病有所增加,然后趋于整体稳定,在年龄≥75年的参与者中持续增加。AF患病率的大幅度增加与房颤相关的合并症的时间变化相关,这表明有必要全面实施房颤预防和管理策略。
心房颤动的发病率和患病率预计将急剧增加,但是,研究人员目前缺乏未被研究选中的临床人群房颤时间趋势的综合数据。近日,心血管疾病领域权威杂志JAHA上针对这一问题发表了一篇研究文章。
在英国的临床实践研究数据(CPRD)分析中,从1998年到2010年期间发生房颤的患者,排除了重大瓣膜疾病患者,与住院资料和全国统计数据相链接。57818名成年人被纳入研究,这些患者平均年龄为74.2岁(SD为11.7),48.3%为妇女。
整体年龄调整后的房颤发病率为每1000人每年在1998-2001年期间为1.11人(95%可信区间为1.09-1.13),在2002-2006年期间为1.33人(1.31-1.34),以及在2007-2010年期间为1.33人(1.31-1.35)。在年龄≥75年的参与者中房颤的发病率不断增加,在男性和女性中具有相似的时间趋势。相关的合并症随着时间的推移而有所变化,既往卒中的患病率不变,而高血压和糖尿病患病率有所增加,缺血性心脏疾病患病率有所降低。年龄在55-74岁的患者中,随着时间变化的死亡率显著降低(P<0.001),但在年龄≥75岁的老年患者中死亡率保持稳定在14%-15%每年(P=0.84)。预测房颤患病率呈逐年上升趋势,预计英国房颤患者将从2010年的700000例患者增加到2060年的13000000-18000000例。
在大型的一般实践人群中,房颤发病有所增加,然后趋于整体稳定,在年龄≥75年的参与者中持续增加。AF患病率的大幅度增加与房颤相关的合并症的时间变化相关,这表明有必要全面实施房颤预防和管理策略。
原始出处:
Deirdre A. Lane, et al. Temporal Trends in Incidence, Prevalence, and Mortality of Atrial Fibrillation in Primary Care.JAHA.2017. https://doi.org/10.1161/JAHA.116.005155
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发病率#
54
#患病率#
56
#AHA#
53
学习了谢谢分享
86
学习过了,值得研究。
0
这个的确是对的
83
学习
68