Sci Rep:膀胱镜下水肿特征提供了间质性膀胱炎治疗后的临床和长期预后特性
2021-01-31 AlexYang MedSci原创
最近,有研究人员评估了间质性膀胱炎/膀胱疼痛综合征(IC/BPS)患者的临床症状、尿动力学参数和长期治疗效果与膀胱镜下水肿(HD)不同结果的相关性。
最近,有研究人员评估了间质性膀胱炎/膀胱疼痛综合征(IC/BPS)患者的临床症状、尿动力学参数和长期治疗效果与膀胱镜下水肿(HD)不同结果的相关性。
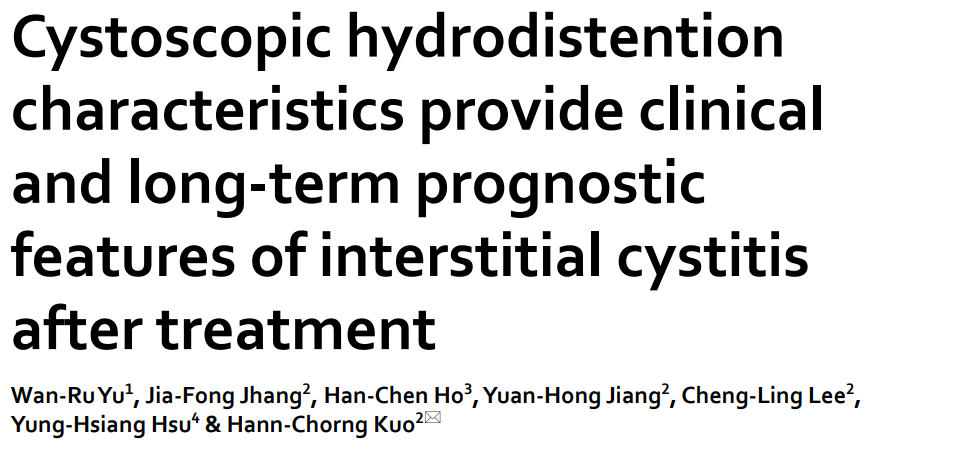
研究包括了486例IC/BPS患者,回顾性分析调查了基线临床症状、病程、医疗合并症、尿动力学结果、膀胱镜特征[包括最大膀胱容量(MBC)和是否存在肾小球和Hunner病变],以及根据肾小球等级、MBC和是否存在Hunner病变的5种IC/BPS HD亚型的治疗结果。研究发现,肾小球等级与MBC显著相关(r=- 0.403,P<0.001),且均与IC症状指数评分显著相关。肾小球等级低、MBC≥760 ml的患者满意率较好(64.2%),Hunner's病变患者的满意率明显较差(36.8%);其他各组间无明显差异。结果表明了IC/BPS患者可分为以下三个不同的亚组。(1)肾小球等级低,MBC≥760ml者;(2)肾小球等级低,MBC<760ml,或无论MBC如何,肾小球等级均高;(3)Hunner's病变者。
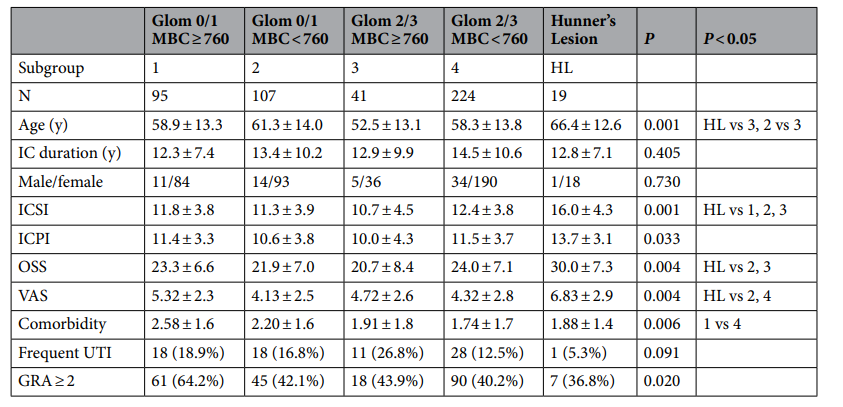
最后,研究人员指出,3个IC/BPS亚组具有明显的膀胱特征和治疗效果。HD后高MBC和低肾小球等级的患者有较多的医学合并症,但治疗效果满意率明显较高。
原始出处:
Wan-Ru Yu, Jia-Fong Jhang, Han-Chen Ho et al. Cystoscopic hydrodistention characteristics provide clinical and long-term prognostic features of interstitial cystitis after treatment. Sci Rep. Jan 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#间质性膀胱炎#
75
#间质性#
71
#长期预后#
71
#水肿#
72