Eur Radiol:用磁共振来评价骨肿瘤的化疗效果并评价生存期
2021-03-13 shaosai MedSci原创
在骨肉瘤中,化疗诱导的肿瘤坏死是公认的预后预测因素。经化疗后肿瘤坏死超过90%患者的生存率明显提高。因此,确立一种能够在手术切除前无创的预测肿瘤对新辅助化疗反应的方法十分有必要。

骨肉瘤(OS)是最常见的原发性恶性骨肿瘤,在儿童和青少年中发病率最高。目前OS的治疗策略是首先行新辅助化疗诱导肿瘤坏死,使其体积缩小后行手术切除。与单纯手术治疗相比,术前和术后联合化疗使患者的长期生存率由20%提高到近70%]。
在骨肉瘤中,化疗诱导的肿瘤坏死是公认的预后预测因素。经化疗后肿瘤坏死超过90%患者的生存率明显提高。因此,确立一种能够在手术切除前无创的预测肿瘤对新辅助化疗反应的方法十分有必要。
磁共振成像(MRI)已成为原发性骨肿瘤诊断和术后肿瘤复发检测的重要手段。DCE-MRI中的容量转移常数(Ktrans)和DW-MRI化疗后的表观扩散系数(ADC)的变化与既往研究的病理反应具有相关性。然而,以往的研究都只关注肿瘤区域的影像学参数的变化,忽略了对肿瘤周围区域的研究。多位学者认为肿瘤附近残留的区域可能是导致治疗失败和局部复发的主要原因。然而现阶段,肿瘤相关的影像学参数是否与肿瘤的进展和治疗效果相关尚不明确。
近日,发表在European Radiology杂志的一项研究评价了OS患者肿瘤和肿瘤周围区域弥散加权成像(DWI)和动态增强磁共振成像(DCE-MRI)的参数,为术前新辅助化疗的肿瘤组织学反应的提供了早期影像学指标并提出了无事件生存期(EFS)和总体生存率(OS)的可能预后因素。
评估骨肉瘤患者方法:本研究纳入了34例OS患者,每位患者均在2014-2018年期间接受了三个疗程的新辅助化疗,然后进行了手术。所有患者均接受基线时以及化疗后的DWI和DCE-MRI扫描。病变区域定义为肿瘤区域和肿瘤周围区域。我们评价了表观扩散系数、容量转移常数(Ktrans)、消除速率常数、血管外细胞外空间体积比(Ve)、曲线下的初始面积以及病变区域化疗前后的相应差异等参数。受试者工作特性曲线分析用于评价这些参数的诊断性能。同时计算了所有参数与肿瘤组织学反应、EFS以及总生存期的关系。
在肿瘤区域,有中等程度的证据表明反应者的post-Ktrans较不良应答者低(p = 0.04,错误发现率[FDR]校正),并且ΔKtrans表现出显着的组间差异(p = 0.04,Bonferroni校正;或p = 0.006,FDR校正)。 在肿瘤周围区域的Ve表现出较弱程度证据的组间差异(治疗前p = 0.025,治疗后p = 0.021,未校正)。此外,肿瘤区域的post-Ktrans降低和肿瘤周围区域的Ve降低是延长EFS(p = 0.002,p = 0.026)和总生存期(p = 0.003,p = 0.023)的重要预后指标。
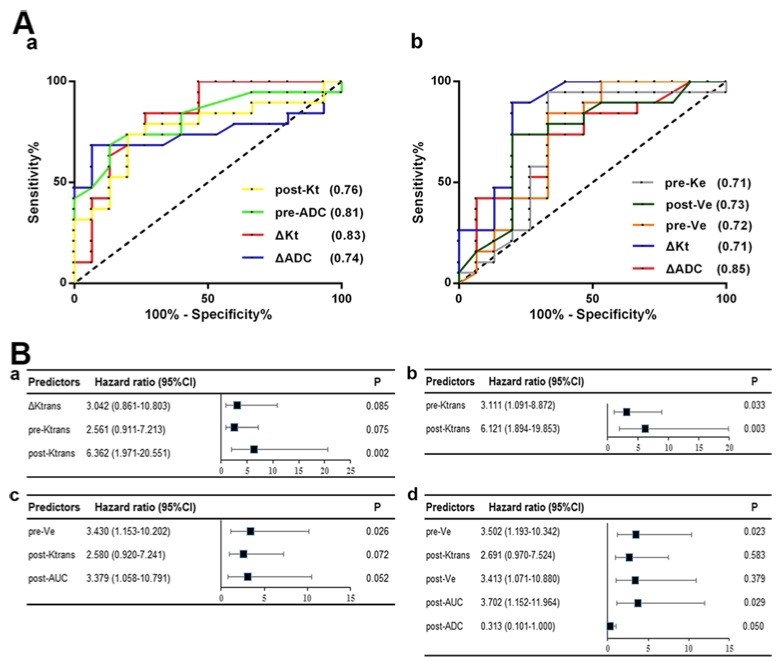
图1 A 肿瘤和瘤周区域参数的ROC曲线。(a)肿瘤区域,(b)瘤周区域。B Cox危险模型用于估计与EFS/总生存率相关的DW-和DCE-MRI参数的危险比和95%置信区间。143/5000
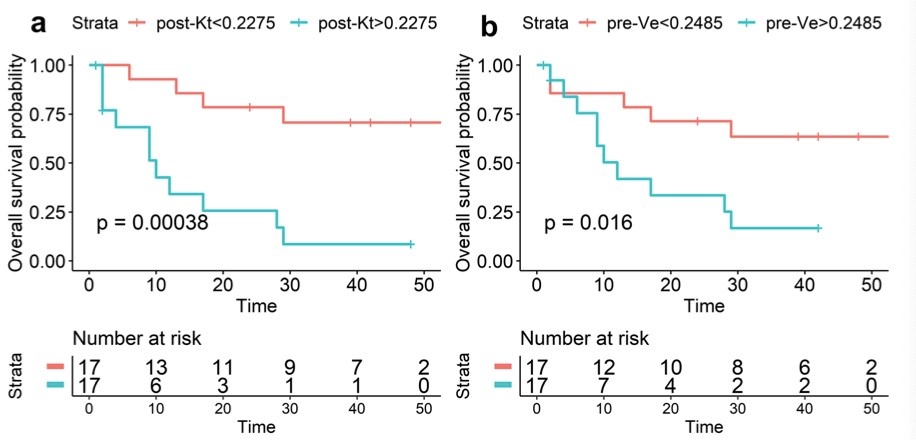
图2 根据肿瘤区域的(a)post-Kt和肿瘤周围区域的(b)pre-Ve 的中位值分层的亚组的无事件生存曲线。
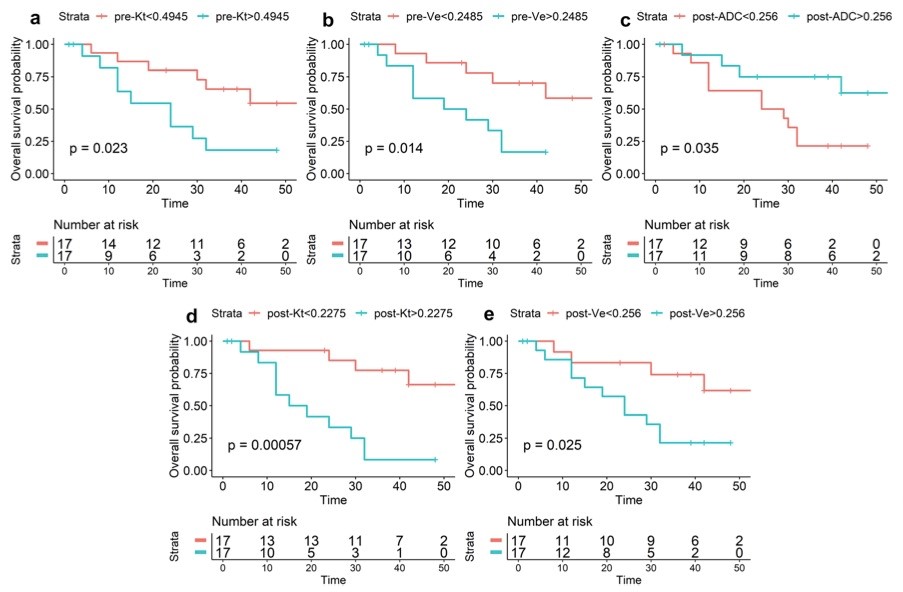
图3 根据肿瘤区域的(a)post-Kt、(b)pre-Ve 及肿瘤周围区域的(c)pre-Ve、(d)post-Ve、(e)post-ADC的中位值分层的亚组的生存曲线。
肿瘤和瘤周区域的DWI和DCE-MRI参数可以反映化疗反应并预测EFS和总生存率,在一定程度上补充和提高了MR成像对OS患者的诊断和预后价值。
原文出处:
Yuewen Hao,Rui An,Yingsen Xue,et al.Prognostic value of tumoral and peritumoral magnetic resonance parameters in osteosarcoma patients for monitoring chemotherapy response. DOI:10.1007/s00330-020-07338-y
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了
122
Mri骨肉瘤研究应用
116
#磁共振#
76
#生存期#
66
#评价#
65
谢谢梅斯提供这么好的信息,学到很多
84
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
88