ESMO世界胃肠癌大会:murlentamab的II期临床研究结果
2019-07-07 Allan MedSci原创
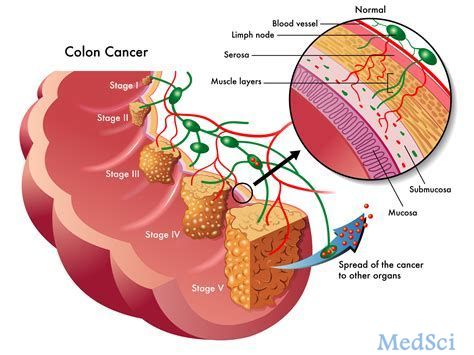
GamaMabs是一家临床阶段生物技术公司,专注于开发抗AMHRII的抗体药物,近日宣布,将在ESMO世界胃肠癌大会上公布murlentamab治疗转移性结直肠癌(mCRC)II期临床数据。
GamaMabs是一家临床阶段生物技术公司,专注于开发抗AMHRII的抗体药物,近日宣布,将在ESMO世界胃肠癌大会上公布murlentamab治疗转移性结直肠癌(mCRC)II期临床数据。
结果显示,murlentamab与trifluridine/tipiracil联用时,PFS率比预期更长(在4个月和6个月时分别为40%和31%)。更令人惊喜的是,在AMHRII阳性肿瘤细胞超过20%的患者中,4个月和6个月时的PFS率分别为83%和75%。murlentamab单药治疗和murlentamab联合trifluridine/tipiracil治疗时,肿瘤生长速率分别下降了1.7倍和3.6倍。
原始出处:
http://www.firstwordpharma.com/node/1651651#axzz5syvQI0kQ
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#II期临床研究#
63
#研究结果#
102
#mAb#
64
#I期临床#
48
#SMO#
68
#ESMO#
86
#II期临床#
53