Acta Neuropathologica: 多发性硬化症再髓鞘化受损的阶段依赖性原因
2020-10-20 MedSci原创 MedSci原创
多发性硬化症(MS)是中枢神经系统最常见的炎症和脱髓鞘疾病,也是导致年轻人残疾的主要原因。它影响到全世界大约230万人,大约50%的患者在患病10-15年后需要助步器。
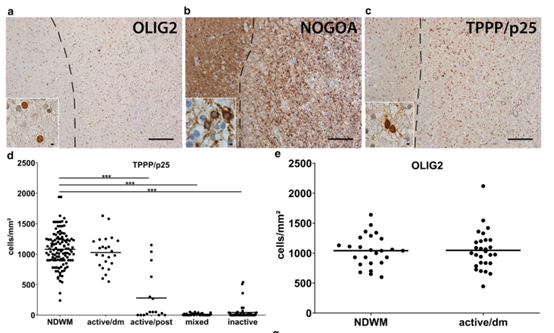
多发性硬化症(MS)是中枢神经系统最常见的炎症和脱髓鞘疾病,也是导致年轻人残疾的主要原因。它影响到全世界大约230万人,大约50%的患者在患病10-15年后需要助步器。在组织病理学上,多发性硬化的特征是多灶性脱髓鞘病变、炎性浸润(巨噬细胞、T细胞和B细胞)、轴突受损和数量减少以及少突胶质细胞缺失。尽管近年来免疫疗法取得了重大进展,但疾病的进展仍然无法阻止。再髓鞘化是指在脱髓鞘后形成新的髓鞘,在多发性硬化病变中可能失败。祖细胞向有髓少突胶质细胞的分化受损可能是再髓鞘化失败的原因,因此,促进少突胶质细胞分化和髓鞘再形成的药理学方法的发展代表了一种有前途的新治疗方法。然而,这一普遍接受的概念最近受到了挑战。
为了进一步了解MS再髓鞘化失败的机制,我们评估了白质中不同MS病变类型中少突胶质细胞的数量、髓鞘再形成的存在以及炎症环境,并使用诱导多能干细胞(iPSC)衍生的少突胶质细胞(hiOL)和极化的人小胶质细胞上清液进行了体外实验。我们的研究结果表明,多发性硬化症的再髓化失败有多种原因,这些原因取决于病变的分期,主要包括:尽管在活动性病变的亚群中存在成熟的少突胶质细胞,但缺乏髓鞘形成;在混合性活动性/非活动性病变中,少突胶质丢失,组织环境恶劣。
方法:本研究回顾性地收集了62例患者的石蜡包埋脑活检和尸检组织标本。队列包括来自32名患者的38个活检组织样本和来自30名患者尸检的113个MS病变(81个组织块)。在尸检中,17名患者的53个组织块(71个病灶)来自明斯特大学医院神经病理学研究所的尸检收集。从荷兰脑库,荷兰神经科学研究所,阿姆斯特丹获得了来自13名患者的具有42个病灶的28个组织块;所有的材料都是从捐赠者那里收集的,这些捐赠者都有脑解剖的书面知情同意书,并且NBB已经获得了用于研究目的的材料和临床信息。脑活检是显示非典型磁共振成像结果的不清楚单病灶诊断评估的一部分。研究作者中没有人参与活检或尸检的决策。这项研究得到了明斯特大学和麦吉尔大学伦理委员会的批准。
综上所述,我们认为,要成功地开发出促髓再生药物,就需要有更好的体内和体外模型来模拟不同类型的MS病变的病理特征。
Heß, K., Starost, L., Kieran, N.W. et al. Lesion stage-dependent causes for impaired remyelination inMS. Acta Neuropathol 140, 359–375 (2020). https://doi.org/10.1007/s00401-020-02189-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Pathol#
41
#髓鞘#
72
#多发性#
54
#pathologic#
50
#硬化症#
44
#CTA#
50