Carcinogenesis:TAZ诱导乳腺癌机制被破解
2012-01-06 MedSci原创 MedSci原创
近日,国际癌症领域主流杂志Carcinogenesis刊登了中国科学院昆明动物研究所研究人员的最新研究成果“TAZ antagonizes the WWP1-mediated KLF5 degradation and promotes breast cell proliferation and tumorigenesis。”文章中,研究人员首次证实了TAZ促进乳腺细胞的增生机制是部分通过保护KLF
近日,国际癌症领域主流杂志Carcinogenesis刊登了中国科学院昆明动物研究所研究人员的最新研究成果“TAZ antagonizes the WWP1-mediated KLF5 degradation and promotes breast cell proliferation and tumorigenesis。”文章中,研究人员首次证实了TAZ促进乳腺细胞的增生机制是部分通过保护KLF5免受WWP1介导的泛素化降解。
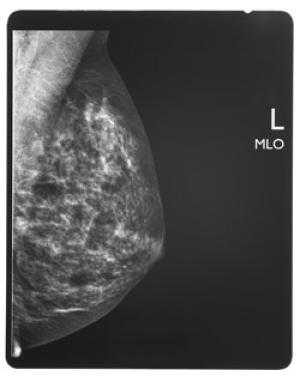
乳腺癌是女性最常见的恶性肿瘤之一,雌激素受体ER、孕激素受体PR和表皮生长因子受体HER2均为阴性的(简称三阴性)乳腺癌是预后最差的一类,目前没有有效的靶向治疗药物,对放射治疗和化疗也不敏感,因此寻找三阴性乳腺癌的有效治疗靶点是目前研究的热点之一。中国科学院昆明动物研究所肿瘤生物学实验室陈策实研究员领导的学科组前期研究显示KLF5转录因子在一部分三阴性的乳腺癌中特异高表达,KLF5通过紧密控制FGF-BP癌基因表达促进细胞增殖、生存以及肿瘤生长,WWP1 E3泛素连接酶促进KLF5蛋白的降解并抑制其功能,但是KLF5的正向调控机制尚不清楚。
最近,中国科学院昆明动物研究所肿瘤生物学实验室陈策实研究员博士后赵东等人,通过一系列实验研究发现, Hippo肿瘤抑制信号途径的TAZ(transcriptional co-activator with a PDZ-binding motif)癌蛋白通过其WW结构域结合KLF5的PPXY序列,拮抗WWP1 介导的KLF5的蛋白降解,促进KLF5的下游基因表达、细胞增殖以及肿瘤生长。而抑制TAZ的蛋白激酶LATS1可以通过TAZ抑制KLF5的表达和活性。这项研究首次证实了TAZ促进乳腺细胞的增生机制是部分通过保护KLF5免受WWP1介导的泛素化降解,从而增强KLF5对下游癌基因表达的控制并且促进细胞周期进展。该研究提示KLF5可能是Hippo肿瘤抑制信号途径中的关键下游成员,并且证明KLF5和TAZ可以作为三阴性乳腺癌的潜在治疗靶点。
该项研究得到了国家自然科学基金和云南省高端人才项目支持。(生物谷Bioon.com)
TAZ antagonizes the WWP1-mediated KLF5 degradation and promotes breast cell proliferation and tumorigenesis
Dong Zhao1,2,†, Xu Zhi1,2,†, Zhongmei Zhou1 and Ceshi Chen1,*
Krüppel-like factor 5 (KLF5) is a PY motif-containing transcription factor promoting breast cell proliferation. The KLF5 protein is rapidly degraded through the proteasome after ubiquitination by E3 ubiquitin ligases, such as WWP1 and SCFFbw7. In this study, we demonstrated that a transcriptional co-activator with the PDZ binding motif (TAZ) upregulated the KLF5 expression through antagonizing the WWP1-, but not Fbw7-, mediated, KLF5 ubiquitination and degradation. TAZ interacted with KLF5 through the WW domain of TAZ and the PY motif of KLF5, which is the binding site for WWP1. TAZ inhibited WWP1-KLF5 protein interaction and WWP1-mediated KLF5 ubiquitination and degradation in a WW domain dependent manner. Overexpression of TAZ up-regulated the protein levels of KLF5 and FGF-BP, which is a well established KLF5 target gene. In addition, depletion of TAZ in both 184A1 and HCC1937 breast cells down-regulated protein levels of KLF5 and FGF-BP and inhibited cell growth. Furthermore, stable depletion of either TAZ or KLF5 significantly suppressed HCC1937 xenograft growth in immunodeficient mice. Knockdown of LATS1, a TAZ upstream inhibitory kinase, up-regulated the protein levels of KLF5 and FGF-BP in 184A1 and promoted cell growth through TAZ. Finally, both KLF5 and TAZ were co-expressed in a subset of estrogen receptor (ERα)-negative breast cell lines. These results, for the first time, suggest that TAZ promotes breast cell growth partially through protecting KLF5 from WWP1-mediated degradation and enhancing KLF5’s activities.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AZ#
68
#CIN#
48
#Carcinogenesis#
65
#Gene#
64
#ESI#
63