JACC:IL-1β对急性失代偿心衰患者预后的预测价值
2019-03-20 不详 MedSci原创
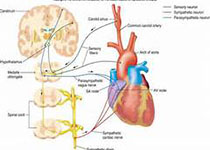
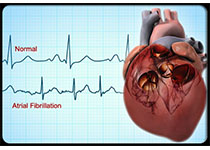
可溶性ST2(sST2)是白介素(IL)-1受体样-1的一种形式,可以预测急性失代偿心衰(ADHF)的风险。 IL-1β是一个对心肌重塑和功能有害的炎症因子,急性心梗后 IL-1β抑制剂的应用可以改善预后,然而, IL-1β与ADHF和sST2的相关性尚不明确。本研究的目的旨在评估IL-1β与sST2的相关性,及其对ADHF患者的预后价值。本研究纳入了316名因ADHF住院的患者(平均年龄为72±
Domingo A et al.The Interleukin-1 Axis and Risk of Death in Patients With Acutely Decompensated Heart Failure.JACC 2019 Mar.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
80
#患者预后#
69
#ACC#
80
#心衰患者#
81
#IL-1β#
88
#IL-1#
81
#预测价值#
86