NEJM:感染性休克患者早期靶向治疗效果如何?
2017-03-22 xing.T MedSci原创
在这项对个体病人数据进行的荟萃分析中,EGDT并不会比常规治疗产生更好的结局,并且与所有特点的患者和医院的较高住院费用有关。
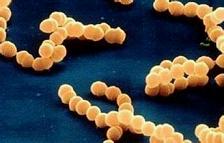
在一个单中心临床试验和观察性研究提示早期目标导向治疗(EGDT)可以降低感染性休克死亡率后,三个多中心试验(ProCESS、ARISE和ProMISe)显示无效益。最近,顶级医学期刊NEJM上发表了一篇荟萃分析文章,研究人员对最近的三个前瞻性试验的个体患者数据进行荟萃分析,以提高统计效能并探索EGDT治疗效果的异质性。
研究人员统一了研究准入标准、干预方案、结局、资源利用的指标、并通过试验数据的收集,并在揭盲前明确所有分析。试验完成后,研究人员汇总了数据,排除了ProCESS研究基于协议的标准治疗组,并分析残留差异。该研究的主要结局为90天死亡率。次要结局包括1年生存率、器官支持和住院费用。研究人员检验了16个病人的特点的治疗亚组相互作用和6个护理服务特性。
研究人员分析了七个国家138家医院的3723名病人。研究人员发现90天的死亡率在EGDT治疗组(1852例中的462例[24.9%])和常规治疗组(1871例中的475例[25.4%])相似;调整后的比值比为0.97(95%可信区间为0.82-1.14;P=0.68)。EGDT相比于常规治疗与较高的平均(±SD)使用重症监护(5.3±7.1 vs. 4.9±7天,P=0.04)和心血管支持(1.9±3.7 vs. 1.6±2.9天,P=0.01)有关;而其他的结局没有显著差异,尽管EGDT治疗的平均成本较高。亚组分析显示休克更严重的患者(高血清乳酸水平,合并低血压和高乳酸血症,或更高的死亡预测风险)或复苏期间使用升压药或液体治疗倾向性较低的医院并没有从EGDT治疗中获得效益。
在这项对个体病人数据进行的荟萃分析中,EGDT并不会比常规治疗产生更好的结局,并且与所有特点的患者和医院的较高住院费用有关。
原始出处:
Giovanni Landoni, et al. Early, Goal-Directed Therapy for Septic Shock — A Patient-Level Meta-Analysis. N Engl J Med 2017; http://www.nejm.org/doi/full/10.1056/NEJMoa1616325#t=abstract
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗效果#
51
#感染性#
45
学习了,谢谢!
0
谢谢指点迷津
83
学习了
68
很好的学习资料,谢谢了。
88
学习了!!!
89
学习了
49