多发性硬化症(MS)的疾病过程以炎症和神经变性为特征。所有形式的多发性硬化症的共同点是大脑和脊髓的炎症病灶,这些病灶可以通过磁共振成像显示出来。这些病灶内活跃的炎症性脱髓鞘导致血脑屏障受损,因此活跃的脱髓鞘病灶可以用钆基对比剂来识别。MRI扫描上的对比剂增强病变(contrast enhancing lesion, CELs)表明在扫描时有活跃的炎症性脱髓鞘,因此被视为当前炎症性疾病活动的可靠的放射学生物标志物。在RRMS试验中,CEL的存在和数量是一个重要的次要结果,但CEL在MS的所有疾病过程中都会发生。
一些研究显示,CEL的频率随着年龄的增长而降低,这一发现与复发随年龄和疾病持续时间减少的观察一致,也与MS的炎症性疾病活动在年轻人中更明显,在老年人中更不普遍的一般观点一致。然而,这些研究以RRMS患者为主,不太清楚观察到的年龄和CEL发生的关联是否存在于所有MS疾病过程中。
藉此,加拿大University of Calgary的Marcus W. Koch等人,使用了四个大型随机对照试验(RCTs)的数据集,包括复发缓解型多发性硬化症(RRMS)、继发性进展型多发性硬化症(SPMS)和原发性进展型多发性硬化症(PPMS),以探究年龄与基线和实验性治疗一年后出现CELs的关系。
他们利用CombiRx队列的原始试验数据,即RRMS的试验,ASCEND的SPMS试验,以及PROMISE和INFORMS两项初级进展型多发性硬化症的试验,描述整个试验队列基线时和治疗组一年后的各年龄组CEL发生情况。
CombiRx包括1,008人,ASCEND 889人,PROMISE 943人,INFORMS 970人。
在基线时,CEL的频率在不同的数据集中因疾病过程而不同。39.6%的CombiRx、23.9%的ASCEND、14.0%的PROMISE和12.3%的INFORMS参与者有CELs。
这种按病程的分布在每个年龄组内基本保持不变。
在所有的数据集中,随着年龄的增长,患有CELs的参与者的比例几乎呈线性下降。
实验性治疗一年后,所有试验数据集的CEL发生率都有所下降,在ASCEND中几乎没有。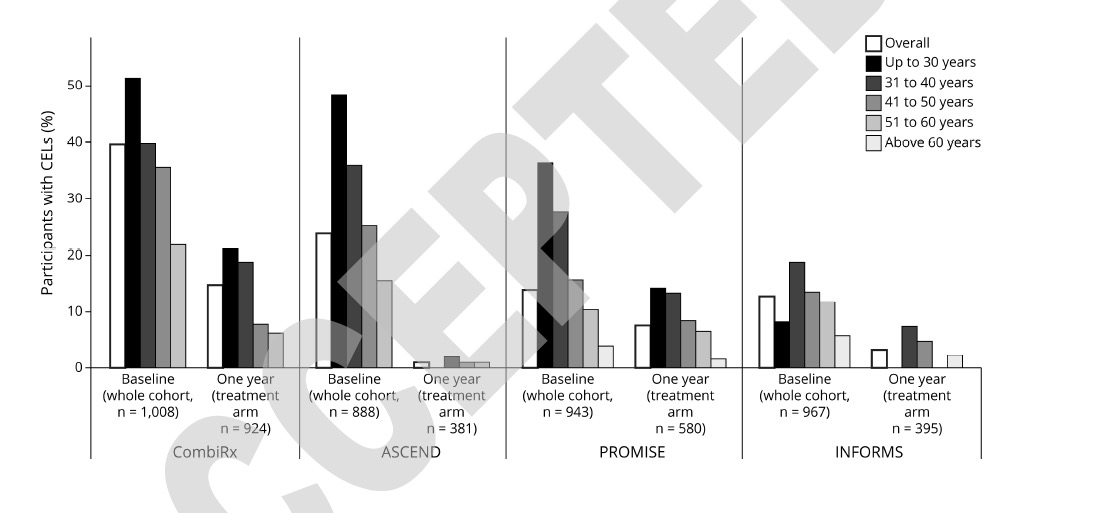
在CombiRx、PROMISE和INFORMS中,随着年龄的增长,CEL发生率的下降在一年的治疗后得以保留。
在所有数据集中,年龄是唯一与基线CELs风险相关的特征,年龄越大,CELs的风险越低(年龄每增加一岁,基线上有CELs的几率(OR)。
这个研究的重要意义在于发现了:对四个大型的、特征明确的RCT数据集的分析表明,年龄和CEL的发生是整个MS疾病过程中的一个普遍现象。这个研究结果,应该能在现实世界的多发性硬化症数据集中得到验证。
原文出处:
Koch MW, Mostert J, Zhang Y, et al. Association of Age With Contrast-Enhancing Lesions Across the Multiple Sclerosis Disease Spectrum [published online ahead of print, 2021 Aug 10]. Neurology. 2021;10.1212/WNL.0000000000012603. doi:10.1212/WNL.0000000000012603
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Neurol#
81
#多发性#
66
#损伤#
84
学习了
103
学习了
96