后天性膝外翻合并前交叉韧带损伤1例
2019-07-23 许振东 宫良丰 李庆 临床骨科杂志
患者,女,52岁,走路扭伤致左膝关节呈屈曲外翻位,当时出现肿胀,听到弹响,于2017年8月25日急诊入院。查体:左膝关节呈屈曲外翻畸形,略肿胀,周围无红肿,皮温正常,关节屈伸活动度10°~100°,过伸痛(-),过屈痛(+),浮髌试验(-),磨髌试验(-),内侧关节间隙压痛(+),外侧关节间隙压痛(-),外翻应力试验(-),前抽屉试验(+),后抽屉试验(-),Lackman试验(+),麦氏试验(-
临床资料
患者,女,52岁,走路扭伤致左膝关节呈屈曲外翻位,当时出现肿胀,听到弹响,于2017年8月25日急诊入院。查体:左膝关节呈屈曲外翻畸形,略肿胀,周围无红肿,皮温正常,关节屈伸活动度10°~100°,过伸痛(-),过屈痛(+),浮髌试验(-),磨髌试验(-),内侧关节间隙压痛(+),外侧关节间隙压痛(-),外翻应力试验(-),前抽屉试验(+),后抽屉试验(-),Lackman试验(+),麦氏试验(-)。患者小时候左膝曾有外伤史。术前X线片(图1A):损伤累及骺板,造成膝外翻。术前双下肢全长X线片测量(图1B):股胫角158°,远端股骨外侧角63°。此次受伤伤及前交叉韧带,关节不稳症状明显,有创伤性关节炎疼痛症状。术前膝关节Lysholm评分46分。
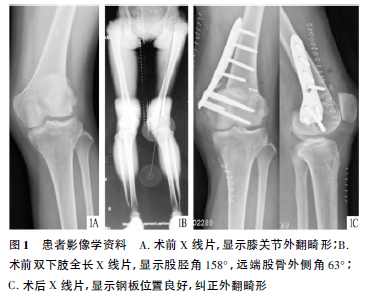
4d后于联合阻滞麻醉下行左股骨闭合楔形截骨术+前交叉韧带重建术。术中根据截骨模块(截骨角度为63°,厚度为3.5cm,截骨平面位于髌骨上缘)进行截骨,恢复下肢力线后行前交叉韧带重建术,胫骨侧采取生物带鞘螺钉挤压,股骨侧采取锁扣带袢钛板,取自体半腱肌与股薄肌进行重建,见图1C。切口一期愈合。前抽屉试验(-),Lackman试验(-)。术后随访3个月,1个月时膝关节屈伸活动度为0°~90°,Lysholm评分86分;2个月时膝关节屈伸活动度为0°~110°,Lysholm评分92分;3个月时膝关节屈伸活动度为0°~125°,Lysholm评分95分。
原始出处:
许振东,宫良丰,李庆.后天性膝外翻合并前交叉韧带损伤1例[J].临床骨科杂志,2019,22(03):277.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#膝外翻#
94
#损伤#
105
#前交叉韧带#
108
#韧带#
100