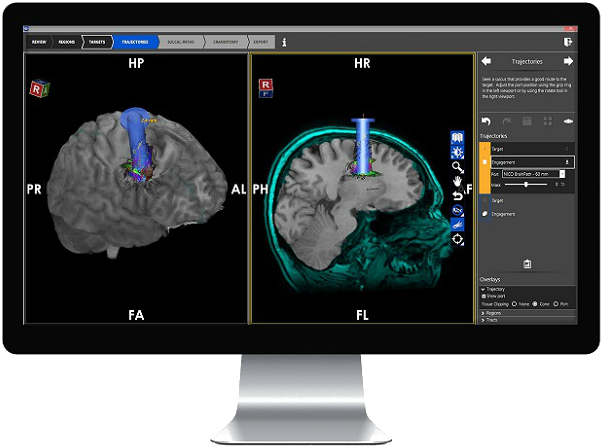
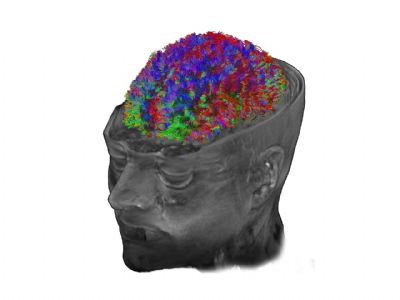
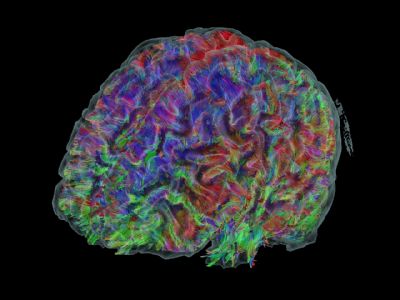
看Synaptive Medical如何颠覆神经外科手术
2015-06-12 徐青 健康界
相信大多数神经外科的医生都有过这样的经历,在培训时面对大脑图表或模型,复杂的结构可以一目了然:额前皮质储存长期记忆,小脑掌管平衡,顶叶整合感觉信息等。但是,当实际进行开颅手术时可完全不是这么一回事,只看到浆糊一样的一团,瞬间背得滚瓜烂熟的规则就全忘了。而脑部手术对精确度要求又极高,下刀位置相差一毫米就有可能永远损坏一名患者的听力、语言能力、行动能力或感觉能力。在现有条件下,神经外科医生在真正手术前



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









神经外科是该进步了!
94
#神经外科手术#
74
#DIC#
0
手术技术进步依赖科技
134
收藏
192
腻害
144
时代在进步
131
牛
85
牛
105
看看
101