乳腺癌新药Ibrance III期临床一线治疗ER+/HER2-乳腺癌获得成功
2016-04-21 佚名 生物谷
美国制药巨头辉瑞(Pfizer)近日公布了突破性乳腺癌药物Ibrance(palbociclib)一项III期PALOMA-2临床研究的积极顶线数据。该研究在既往未接受系统疗法治疗晚期病情的雌激素受体阳性(ER+)、人类表皮生长因子受体2阴性(HER2-)、晚期或转移性乳腺癌绝经后女性患者中开展,数据显示,与来曲唑(letrozole)+安慰剂相比,Ibrance+来曲唑组合疗法显著延长了无进展生
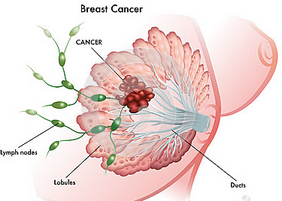
美国制药巨头辉瑞(Pfizer)近日公布了突破性乳腺癌药物Ibrance(palbociclib)一项III期PALOMA-2临床研究的积极顶线数据。该研究在既往未接受系统疗法治疗晚期病情的雌激素受体阳性(ER+)、人类表皮生长因子受体2阴性(HER2-)、晚期或转移性乳腺癌绝经后女性患者中开展,数据显示,与来曲唑(letrozole)+安慰剂相比,Ibrance+来曲唑组合疗法显著延长了无进展生存期(PFS),达到了研究的主要终点。安全性方面,PALOMA-2研究中Ibrance+来曲唑联合治疗组中所观察到的不良事件与Ibrance在横跨不同患者群体及多线治疗中的已知安全性一致。Ibrance用药相关的警告及注意事项包括中性粒细胞减少症、肺栓塞、胚胎毒性。
该研究为Ibrance+来曲唑组合疗法一线治疗晚期乳腺癌提供了确凿的疗效证据,辉瑞此前在II期PALOMA-1研究中对该组合进行了首次研究。这些数据将支持Ibrance进一步的全球监管申请,而在美国市场,这些数据将用于支持Ibrance由加速批准转为完全批准。PALOMA-2研究的详细疗效和安全性数据将提交至2016年美国临床肿瘤学会(ASCO 2016)年度会议。
值得一提的是,PALOMA-2研究也标志着证实Ibrance联合激素疗法治疗ER+/HER2-晚期乳腺癌具有积极疗效的第三个随机研究。在该领域,Ibrance仍然是唯一一种已获得III期临床数据的CDK4/6抑制剂。
Ibrance:将主导HER2-乳腺癌市场,2023年销售额达到18.5亿美元
Ibrance是全球上市的首个CDK4/6抑制剂,于2015年2月获FDA加速批准,联合诺华肿瘤学药物Femara(letrozole,来曲唑)用于既往未接受过系统治疗以控制晚期病情的绝经后女性HR+/HER2-晚期或转移性乳腺癌的一线治疗。
今年2月,FDA进一步批准Ibrance联合阿斯利康肿瘤学药物Faslodex(fulvestrant,氟维司群),用于接受内分泌治疗后病情进展的HR+/HER2-晚期或转移性乳腺癌女性患者的治疗。此次批准,也标志着Ibrance治疗HR+/HER2-乳腺癌成功由一线治疗扩大至二线治疗,将显著扩大Ibrance的患者群体。
业界对Ibrance的商业前景也十分看好。此前,全球医药行业调研机构GlobalData发布报告指出,肿瘤学巨头罗氏(Roche)新推出的2种乳腺癌药物Perjeta和Kadcyla将助其继续称霸HER2+乳腺癌市场;辉瑞将凭借CDK4/6抑制剂Ibrance主导HER2-乳腺癌市场,该药在2023年的销售额将达到18.5亿美元;而阿斯利康将借助PARP抑制剂Lynparza主导三阴乳腺癌(TNBC)市场。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#HER2-#
73
#I期临床#
65
#临床一线#
63
深度好文,值得关注
93
#III#
68
曲伐快不用了吧
219
学习啦
121
新药吗?新东西。
146
未来会统治这个领域!
158
价格多少
102