J Stroke Cerebrovasc Dis: 脑实质血肿2型与缺血性卒中溶栓后24h恶化相关
2016-06-22 MedSci MedSci原创
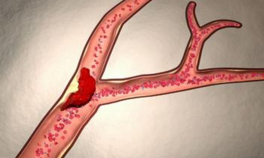
背景:静脉溶栓治疗可以改善急性缺血性卒中(AIS)神经功能预后,但存在出血性转化(HT)的风险。症状性脑出血(ICH)的目前的定义:有一定程度的相关的神经系统恶化。然而,早期继发性脑出血的有害影响,也可能表现为减少神经系统功能的改善。本研究旨在探讨是不同的影像类型的HT和溶栓后24小时神经功能改善程度之间是否独立相关。方法:这项研究是对AIS溶栓病例的中心数据库进行回顾性分析。校正潜在的混杂因素后
背景:静脉溶栓治疗可以改善急性缺血性卒中(AIS)神经功能预后,但存在出血性转化(HT)的风险。症状性脑出血(ICH)的目前的定义:有一定程度的相关的神经系统恶化。然而,早期继发性脑出血的有害影响,也可能表现为减少神经系统功能的改善。本研究旨在探讨是不同的影像类型的HT和溶栓后24小时神经功能改善程度之间是否独立相关。
方法:这项研究是对AIS溶栓病例的中心数据库进行回顾性分析。校正潜在的混杂因素后,应用多元回归分析探讨不同亚型的HT与溶栓后24小时NIHSS评分变化之间的相关性。
结果:与无HT的患者相关,继发ICH亚型脑实质内血肿2型(PH2)与改善减少或NIHSS评分恶化相关,平均效应量为7点(95%CI:-10到14)。在无pH2的情况下,AIS溶栓治疗与24小时内的神经功能改善相关。
结论:HT的PH2型与减少神经功能改善或溶栓治疗AIS后24小时恶化相关。
原始出处:
Gill D, Baheerathan A, et al. Severe Hemorrhagic Transformation after Thrombolysis for Acute Ischemic Stroke Prevents Early Neurological Improvement. J Stroke Cerebrovasc Dis. 2016 Jun 15.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#缺血性卒#
56
#Dis#
50
#缺血性#
50
学习了,好文值得点赞!
76
#ASC#
55
#脑实质#
68
#血肿#
61