Arthritis Rheumatol:系统性硬化症患者的舒张功能障碍的危险因素和对死亡率的影响
2021-12-24 MedSci原创 MedSci原创
DD与SSc患者死亡风险增加独立相关。医务人员应在SSc患者中解决潜在的可改变危险因素,包括CAD和肥胖症,以降低患者死亡风险。
近日,风湿免疫学领域权威杂志Arthritis & Rheumatology上发表了一篇研究文章,该研究旨在明确系统性硬化症(SSc)患者舒张功能障碍(DD)的独立危险因素,并评估DD对SSc患者死亡率的影响。

研究人员对2006年1月1日至2017年11月11日期间加入约翰霍普金斯硬皮病中心队列的SSc患者至少进行了一个可分析的2D超声心动图(2DE)检查,共计806名参与者。
研究人员前瞻性地获得了DD危险因素和SSc疾病特征,并且通过最近的2DE检查确定了DD有无情况。Logistic回归模型用于评估临床危险因素与DD之间的关联,Cox比例风险模型用于评估生存率。
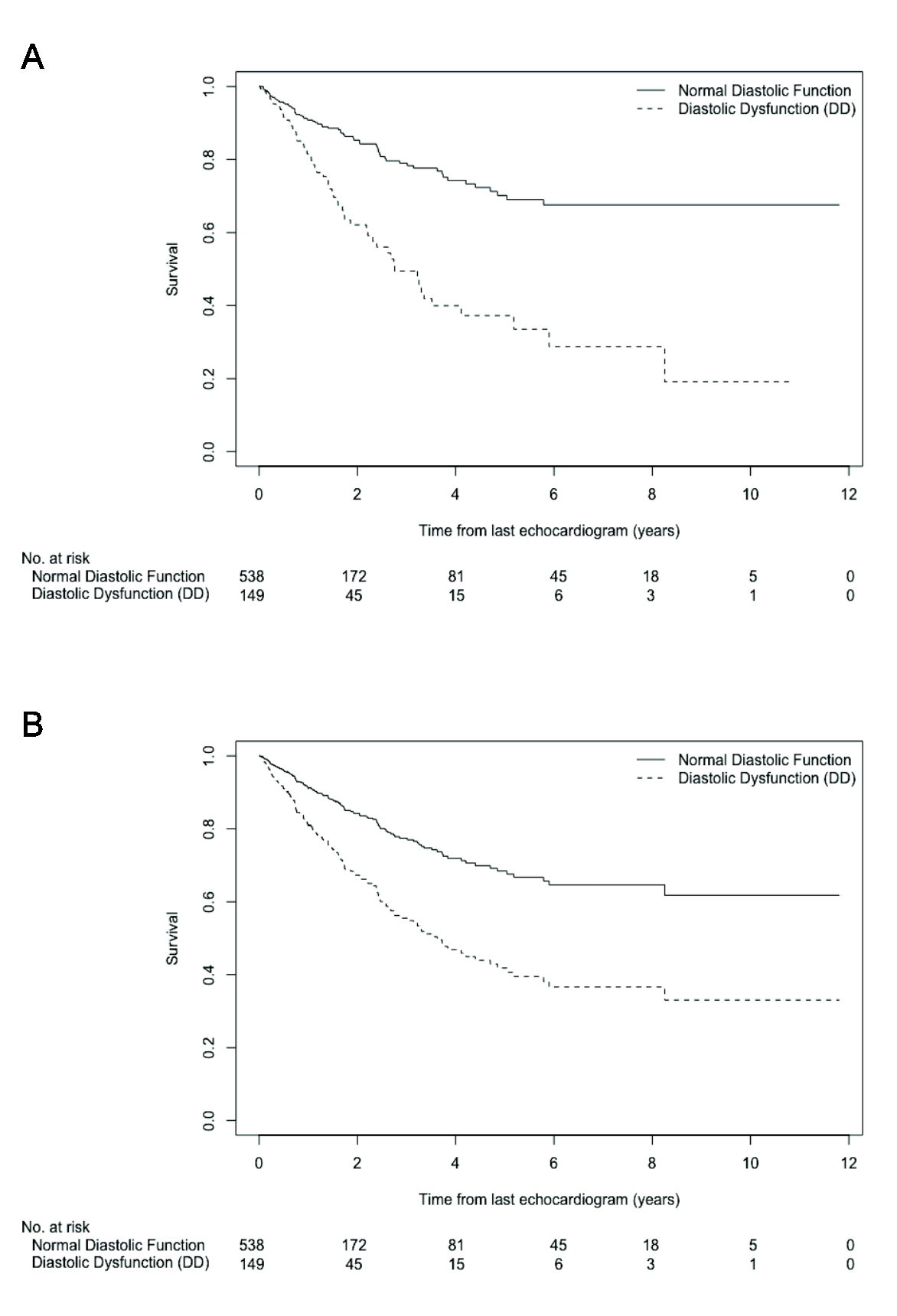
研究人员发现DD存在于18.6%的参与者中。大多数参与者为女性(84%),中位年龄为58.4年(IQR为48.8-68.1)。年龄较大(OR为1.12,95%CI为1.09-1.15)、冠状动脉疾病(OR为3.69,95%CI为1.52-8.97)、肥胖症(4.74,95%CI为2.57-8.74)、SSc病程较长(OR为1.04,95%CI为1.01-1.06)、弥散能力(DLCO)≤预测值的60%(OR为2.41,95%CI为1.40-4.16)和硬皮病肾危象史(OR为3.18,95%CI为1.12-9.07)都是与DD风险增加独立相关。抗Scl70阳性(OR为0.49,95%CI为0.26-0.93)和严重胃肠道疾病(OR为0.48,95%CI为0.30-0.79)与DD风险降低相关。DD的存在与死亡率的增加独立相关(HR为1.69,95%CI为1.07-2.68)。
由此可见,DD与SSc患者死亡风险增加独立相关。医务人员应在SSc患者中解决潜在的可改变危险因素,包括CAD和肥胖症,以降低患者死亡风险。
原始出处:
Alicia M. Hinze,et al.Diastolic Dysfunction in Systemic Sclerosis: Risk Factors and Impact on Mortality.Arthritis Rheumatol.2021.https://onlinelibrary.wiley.com/doi/10.1002/art.42054
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#舒张功能#
130
#Arthritis#
96
#系统性#
70
#舒张功能障碍#
75
#硬化症#
66
#ART#
82
#功能障碍#
68
#系统性硬化#
91