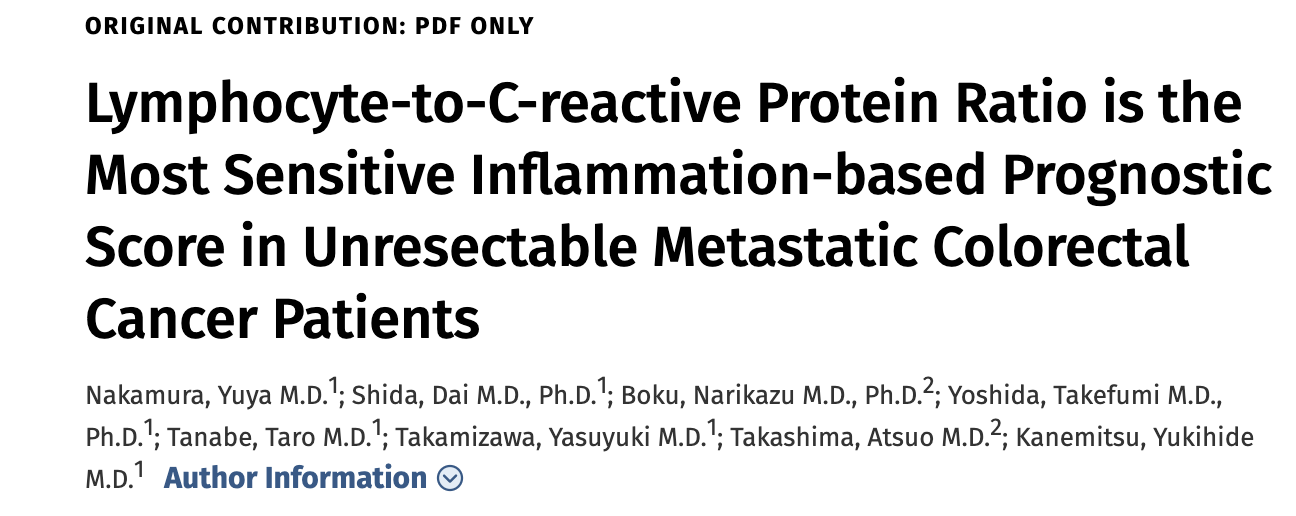
DCR:淋巴细胞与 C 反应蛋白的比率是转移性结直肠癌患者中最敏感的预后指标
2021-06-30 MedSci原创 MedSci原创
我们已经知道全身炎症有助于恶性肿瘤的进展。术前淋巴细胞与 C 反应蛋白的比率最近已被证明可以预测接受手术的结直肠癌患者的生存率
我们已经知道全身炎症有助于恶性肿瘤的进展。术前淋巴细胞与 C 反应蛋白的比率最近已被证明可以预测接受手术的结直肠癌患者的生存率,但其对无法切除的转移性结直肠癌患者的预后价值仍不清楚。因此,本项研究旨在基于炎症的预后评分对淋巴细胞对C反应蛋白的比率与转移性结直肠癌患者的预后进行相关性分析。
这是一项回顾性研究,收集了 2000 年至 2015 年间756 名接受全身化疗的不可切除的转移性结直肠癌患者。通过单变量和多变量分析评估淋巴细胞与 C 反应蛋白比率的预后价值,然后进行了时间依赖的受试者工作特征曲线分析,以比较淋巴细胞与 C 反应蛋白的比率的预后影响与中性粒细胞与淋巴细胞的比率、血小板与淋巴细胞的比率、淋巴细胞与单核细胞的比率或修正格拉斯哥预后评分对于患者预后的预测价值。
研究结果发现高、中和低淋巴细胞-C 反应蛋白患者的中位生存时间分别为 29.4、19.3 和 13.1 个月(p<0.001)。在所有亚组中,患者的预后均可以通过淋巴细胞与C-反应蛋白的比率进行预后分析(体能状态、靶向药物的使用、治疗前癌胚抗原水平、肿瘤侧面、M分类和原发肿瘤切除)。多变量分析显示,淋巴细胞与C反应蛋白的比率降低与存活率降低独立相关(低与高:危险比 1.96,p<0.001;中与高:危险比 1.44,p<0.001)。
本项研究证实淋巴细胞与 C 反应蛋白的比率是不可切除的转移性结直肠癌有用的预后生物标志物,有助于临床医生进行准确的预后判断和治疗决策。
原始出处:
Nakamura, Yuya. Et al. Lymphocyte-to-C-reactive Protein Ratio is the Most Sensitive Inflammation-based Prognostic Score in Unresectable Metastatic Colorectal Cancer Patients. Diseases of the Colon & Rectum.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#淋巴细胞#
75
#预后指标#
89
#转移性#
60
#结直肠#
68