Int J Cardiol:王建安教授发现严重瓣膜疾病中,二尖瓣反流常见
2016-12-07 卢芳 中国循环杂志
疾病也是与时俱进的,为了更好了解当前严重瓣膜性疾病的患病情况,浙江大学附属第二医院王建安等进行了一项医院为基础的调查。结果表明,严重瓣膜性疾病在人群中并不少见,其发病原因在<65岁和≥65岁人群有所差异,前者多为风湿热引起,后者多为退行性病变;前者更多见原发性二尖瓣反流,而后者继发性二尖瓣反流更为多见。 研究显示,在严重瓣膜性心脏病中,二尖瓣反流最为常见,患病率为0.68%;二尖瓣狭窄患
疾病也是与时俱进的,为了更好了解当前严重瓣膜性疾病的患病情况,浙江大学附属第二医院王建安等进行了一项医院为基础的调查。
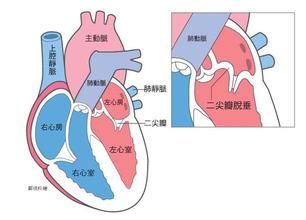
结果表明,严重瓣膜性疾病在人群中并不少见,其发病原因在<65岁和≥65岁人群有所差异,前者多为风湿热引起,后者多为退行性病变;前者更多见原发性二尖瓣反流,而后者继发性二尖瓣反流更为多见。
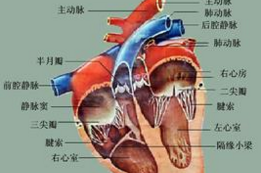
研究显示,在严重瓣膜性心脏病中,二尖瓣反流最为常见,患病率为0.68%;二尖瓣狭窄患病率为0.38%,主动脉瓣狭窄患病率为0.28%,主动脉反流患病率为0.27%。
而且,随着年龄的增长,二尖瓣反流和主动脉瓣狭窄的患病率显著上升,而二尖瓣狭窄却呈明显下降趋势;主动脉反流则与增龄无相关性。
此外,整体来看,不同年龄组严重瓣膜性心脏病的分布无性别差异;就主动脉反流而言,在男性更为多见,而二尖瓣狭窄在女性更为多见。
值得注意的是,研究显示,有0.67%的人罹患严重主动脉瓣膜病变,但这些患者仅19.3%接受了治疗;此外,共有1.22%的人罹患严重二尖瓣瓣膜病变,但接受治疗者也仅15.5%。而且接受治疗的比例随着增龄而显著增加。
研究者指出,虽然该研究提示中国人群严重瓣膜性疾病的患病率较西方国家相对较低,但中国人群基数大,这意味着患者群较为庞大。而且该研究表明绝大多数严重瓣膜性患者并未接受治疗,而且这部分人群随着年龄的增长扩大。
此外,就严重瓣膜性心脏病的发病原因来看,研究显示风湿热仍是“重头”:99.2%的严重二尖瓣狭窄由此而起;也是导致<65岁患者主动脉狭窄和主动脉反流的重要病因之一。
在严重主动脉狭窄患者中,主动脉钙化是最常见病因,其次是二叶型主动脉瓣畸形,后者在年轻患者中多见。
对于≥65岁的主动脉瓣反流患者而言,绝大多数为退行性病变,且随增龄而增加。在严重二尖瓣反流患者中,有60.7%的患者为原发性病变。这些原发性二尖瓣反流患者中,50%由二尖瓣脱垂引起,其次为风湿性疾病。
这项研究共纳入2010-2015年前来该院就诊的139496例≥18岁的住院和门诊患者。其中严重瓣膜性心脏病定义为:严重主动脉瓣狭窄,最大射流速度或平均射流速度≥4 m/s;最大跨瓣压(△P)≥40 mmHg;严重二尖瓣狭窄,瓣膜面积≤1.5 cm2;严重二尖瓣反流,≥3/4级;严重主动脉瓣反流,≥3/4级。
原始出处:
Hu P1, Liu XB1, Liang J1, Zhu QF1, Pu CX2, Tang MY3, Wang JA4.A hospital-based survey of patients with severe valvular heart disease in China.Int J Cardiol. 2016 Nov 25.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cardiol#
57
#二尖瓣#
58
#反流#
68
#瓣膜#
76
呵呵
92
学习了,谢谢!
109
给力的研究
0
了解。
114
是真的吗?!
91
二尖瓣反流是瓣膜病变中最常见的
58