ESC 2016:无需限制饮食胆固醇?新指南一言不合就“打脸”!
2016-08-31 朝家睦 医学界心血管频道
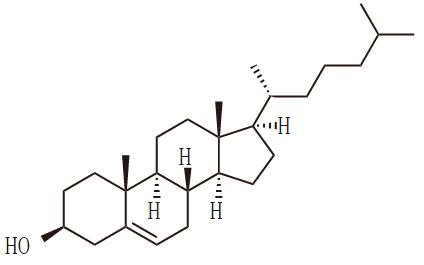
导读:在还热乎的欧洲血脂指南(2016)中,LDL-C依旧稳坐第一把交椅;他的小弟们也跃跃欲试,被分别排了“座次”。LDL-C的“一哥”地位,太牢固了!近来,随着美国居民膳食指南取消之前版本中,推荐的每日摄入胆固醇<300 mg/dL的限制,各种不需限制饮食胆固醇的传言风起云涌,一时间甚嚣尘上。不仅令临床医生困惑,也令广大群众无所适从。于是,反对胆固醇假说的声音再度响起,“降低升高的胆固醇不
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#新指南#
57
文章很好值得关注
81
很好,不错,以后会多学习
0
学学这个
83
继续学习
74
继续关注
68
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
64