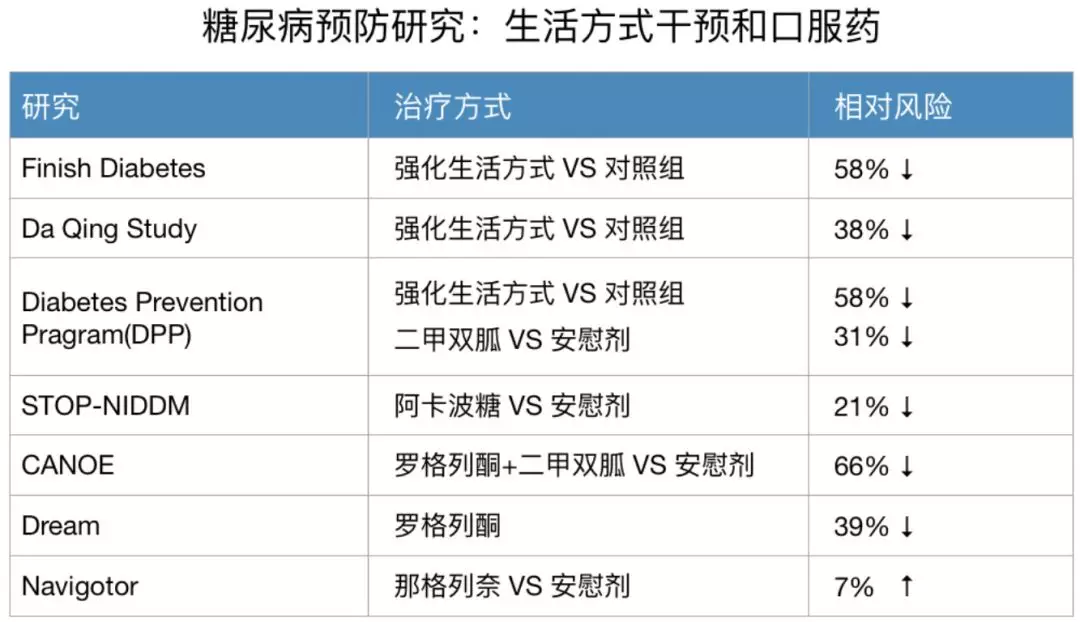
BMJ case report:糖尿病能逆转?间断性“饿”肚子或奏效
2018-10-16 卢芳 中国循环杂志
没有想不到,只有做不到:3个靠吃药打胰岛素控制糖尿病的男士,没有手术,其糖尿病居然逆转了。这是近日刊登在BMJ Case Reports上的活生生的病例。其中,逆转糖尿病的诀窍就是会“饿”肚子,即有计划地去禁食。3位患者年龄在40~67岁,他们平日靠降糖药和胰岛素来控制血糖,此外都有高血压和高胆固醇血症。预计禁食10个月。不过在有计划地科学地“饿”了1个月时,奇迹就出现了:这3个人血糖控制良好,均
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#间断性#
73
#间断#
77
#case report#
75
#BMJ#
51
#case#
86
#Cas#
76
谢谢MedSci提供最新的资讯
0
了解一下,谢谢分享!
110