J Thorac Oncol:德瓦鲁单抗(durvalumab)维持治疗在EGFR和HER2突变不可切除III期NSCLC患者的作用
2021-05-14 yd2015 MedSci原创
德瓦鲁单抗(durvalumab)维持治疗在EGFR和HER2突变不可切除III期NSCLC患者的疗效比较有限,未来需要更多研究探寻这类患者的治疗措施。
PACIFIC研究问世,改写了不可切除III期NSCLC的标准治疗。不可切除III期NSCLC放化疗后无进展患者德瓦鲁单抗(durvalumab)维持治疗4年OS和PFS率分别为49.6% 和35.3%,而对照组为36.3%和19.5%。但是并不是所有的患者都有效。亚组分析发现,EGFR突变的患者没有获益。而且在PACIFIC研究中,只有很少一部分为EGFR突变患者(6%)。因此,德瓦鲁单抗(durvalumab)在EGFR突变患者的疗效不甚明确。近期,来自美国斯坦福大学的研究团队在J Thorac Oncol杂志上发表了一项回顾性研究,评估德瓦鲁单抗(durvalumab)维持治疗在EGFR和HER2突变不可切除III期NSCLC患者的作用。
纳入斯坦福大学肿瘤中心2018年1月1日至2020年3月1日不可切除III期NSCLC放化疗后无进展患者德瓦鲁单抗(durvalumab)维持治疗的患者。相关临床特征被收集。
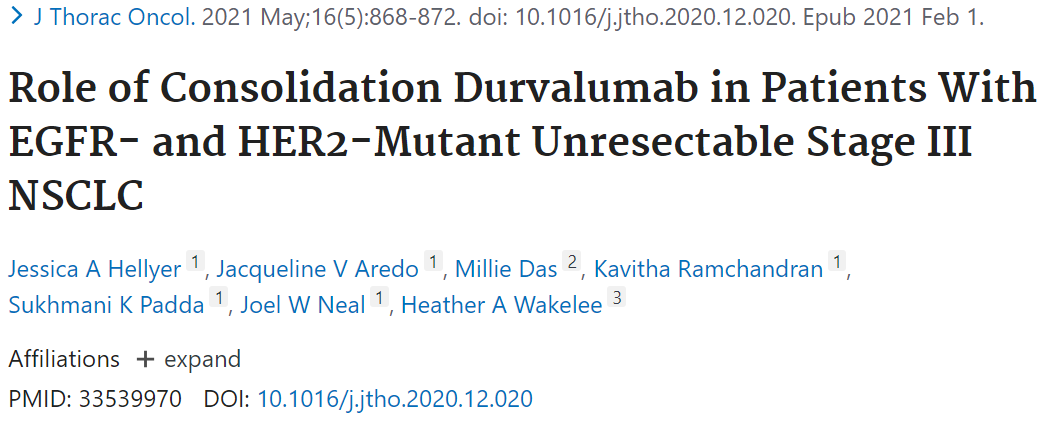
研究共纳入了36例患者,其中11例EGFR 突变 (4例19外显子缺失,1例外显子20插入,6例21外显子L858R突变) 和3例ERBB2外显子20插入突变。ERBB2/EGFR突变组跟ERBB2/EGFR野生组临床特征基本平衡。中位随访时间为14.5个月。
两组的临床特征
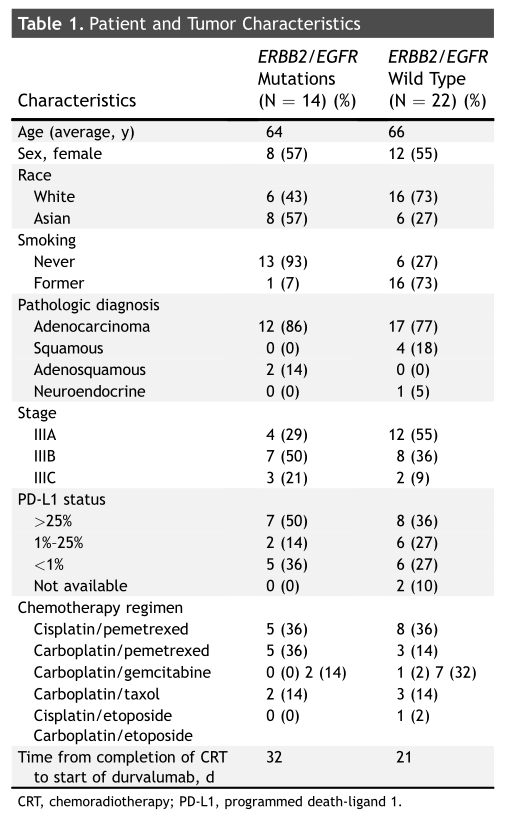
中位无疾病进展生存(DFS):ERBB2/EGFR突变患者为7.5个月,而ERBB2/EGFR野生型患者未达到,HR=2.8,95%CI 1.02-7.67,p=0.04。截止数据分析时,两组中位总生存期(OS)均未达到。
两组的DFS
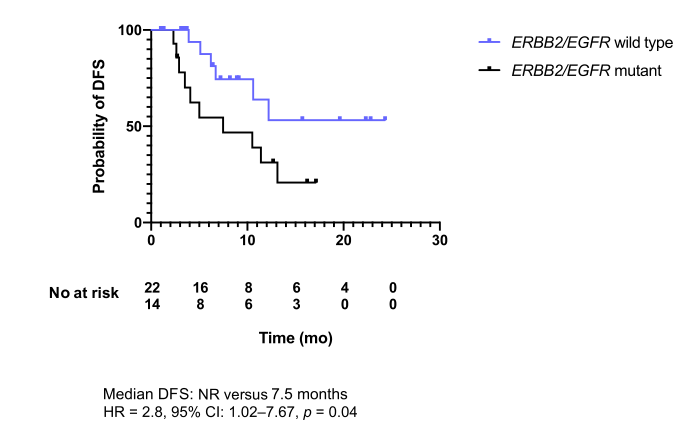
接着,研究者评估PDL1评分对预后的影响。ERBB2/EGFR野生型有2例患者没有进行PD-L1检测被排除分析。总体人群中,PD-L1 <1% 患者的DFS明显短于PD-L1 >1%患者(6.2个月 vs 未达到, p= 0.006)。在ERBB2/EGFR野生型患者中,PD-L1 <1% 患者中位DFS为6.5个月,而PD-L1 >1%患者的DFS未达到,两组有显著统计学差异(p=0.003)。
ERBB2/EGFR野生型PD-L1不同表达水平的DFS
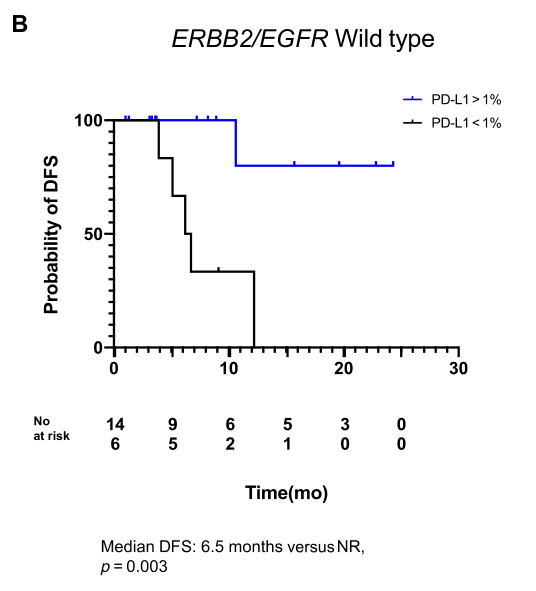
但是,在ERBB2/EGFR突变型患者中,PD-L1 <1% 患者跟PD-L1 >1%患者的DFS没有统计学差异。
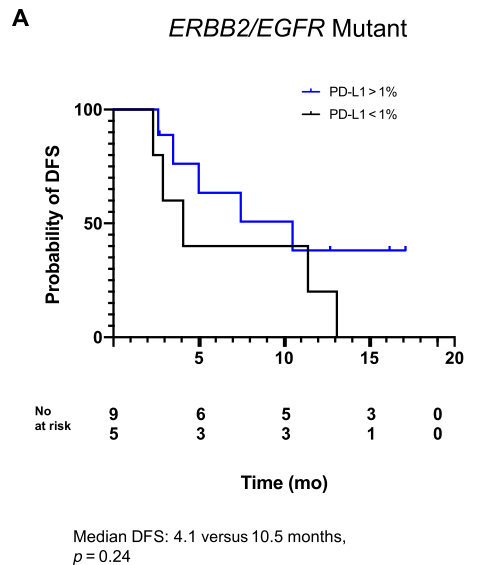
ERBB2/EGFR突变型PD-L1不同表达水平的DFS
最后耐受性评估发现,ERBB2/EGFR突变组中有43%的患者出现免疫相关不良事件,而ERBB2/EGFR野生型组中有59%。ERBB2/EGFR突变组中有4例患者因免疫相关不良反应停止治疗,而ERBB2/EGFR野生型组中有6例患者。
综上,德瓦鲁单抗(durvalumab)维持治疗在EGFR和HER2突变不可切除III期NSCLC患者的疗效比较有限,未来需要更多研究探寻这类患者的治疗措施。
原始出处:
Jessica A Hellyer, Jacqueline V Aredo, Millie Das, et al. Role of Consolidation Durvalumab in Patients With EGFR- and HER2-Mutant Unresectable Stage III NSCLC. J Thorac Oncol. 2021 May;16(5):868-872. doi: 10.1016/j.jtho.2020.12.020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
50
#THORAC#
59
#SCLC患者#
44
#mAb#
56
#III#
59
#NSCLC患者#
62
#GFR#
59
#III期#
49
JTO上有很多不错的好文章,谢谢梅斯及时上新
76
谢谢梅斯分享这么多精彩信息
73