王杰军——深刻认识肿瘤治疗:a person in pain not pain in person
2016-06-18 MedSci MedSci原创
第十二届全国癌症康复与姑息医学大会,于2016年6月17日~19日在合肥举行。本届大会的主题是“科学、人文、实践、合作”。梅斯医学作为媒体合作单位采访了大会主席王杰军教授,以下为部分现场报告。 据统计,美国2015年新发肿瘤例数为166万,死亡病例为59万;而2015年中国癌症发病率和死亡率持续上升,根据《2015年中国癌症统计报告》,中国预计有429.2万例新发肿瘤病例和281.4万例死亡
第十二届全国癌症康复与姑息医学大会,于2016年6月17日~19日在合肥举行。本届大会的主题是“科学、人文、实践、合作”。梅斯医学作为媒体合作单位采访了大会主席王杰军教授,以下为部分现场报告。
据统计,美国2015年新发肿瘤例数为166万,死亡病例为59万;而2015年中国癌症发病率和死亡率持续上升,根据《2015年中国癌症统计报告》,中国预计有429.2万例新发肿瘤病例和281.4万例死亡病例。沉重的数据告诉我们,大多数癌症仍不可治愈,且癌症逐渐向慢性病转化,因此应加大肿瘤的姑息治疗宣传教育,规范肿瘤姑息治疗,最大程度的让患者和家属获益。
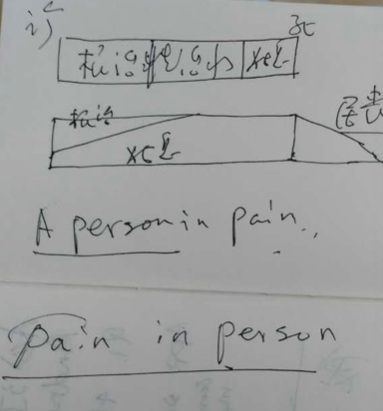
比如,疼痛的治疗首先应理解为一个人患有疼痛,而不是疼痛发生在人身上。人才是治疗的主体,姑息治疗要将人(个体)放在第一位。
人类文明的进步在某个侧面似乎正体现在对每个个体的更大程度的尊重上。而当今医学的发展,尤其是在肿瘤治疗领域,这一趋势表现的尤为突出。大量的研究显示,个体基因及蛋白水平的差异与肿瘤的发生、发展、对治疗的敏感性等均存在着密切的联系。肿瘤的治疗正从传统的同疾则同治的经验模式向量“体”裁“医”的个体化治疗模式转变。这种模式使得疾病的治疗更加注重个体化差异,即更加注重以人为主体的精准、全程、系统化的综合治疗。
随着社会经济水平的发展,人们对精神层面的需求逐渐升高,肿瘤治疗如何在保证“救命”的同时,更大程度的满足患者及家属的精神需求,狭义上来说是在如何以治愈或延长患者生存期为目的的同时,最大程度的改善患者的生活质量。这是临床医生需要不断思考和探索的。这对缓和医患关系也有积极的作用。
总结:大多数肿瘤仍属于不可自愈性疾病,且肿瘤逐渐向慢性病发展,肿瘤患者及家属都有着很大的心理负担,如何保证延长患者生存期的同时,改善生活质量是临床医生需要不断努力的。因此肿瘤患者的姑息治疗至关重要。临床医生应贯彻以人为本的治疗思路,让患者和家属最大程度的获益。

王杰军,教授,医学博士,博士研究生导师,毕业于第二军医大学,现任长征医院肿瘤科主任。中国人民解放军肿瘤专业委员会主任委员、中华医学会上海分会肿瘤专科委员会前任主任委员、中国生命关怀协会副会长、上海癌症康复与姑息治疗专业委员会主任委员、中国癌症康复与姑息治疗专业委员会候任主任委员、上海市防癌抗癌事业发展基金会副理事长、中国临床肿瘤协作中心(CSCO)常务委员、中华医学会疼痛学分会常务委员、国家药品监督管理局药物审评委员会委员、解放军肿瘤研究所副所长、上海综合性医院肿瘤防治专业委员会主任委员等。
梅斯医学
梅斯医学(MedSci)是中国领先的医生互联网平台,拥有超过120万注册医生用户,主要从事临床研究、医生继续教育和培训,以及智慧医疗服务,旨在推动和加速临床医生的职业成长,改善医疗质量。
更多全国癌症康复与姑息医学大会内容,请关注梅斯医学APP

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#王杰军#
64
#PE#
55
#ERS#
75
说的好
130
#肿瘤治疗#
54
好文章,值得学习
187
重视癌症的全程管理和控制
180
领悟了
127
理解的很好,表达的很好
112