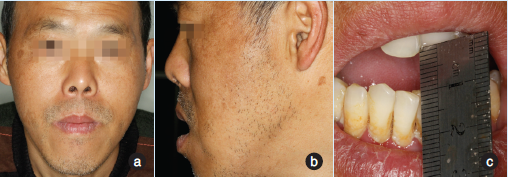
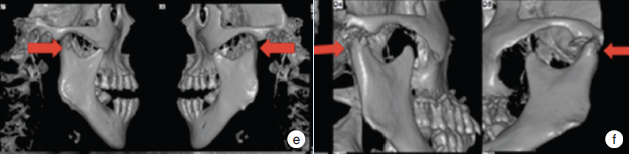
手术治疗陈旧性颞下颌关节脱位1例
2020-01-20 余念 鲁勇 口腔疾病防治
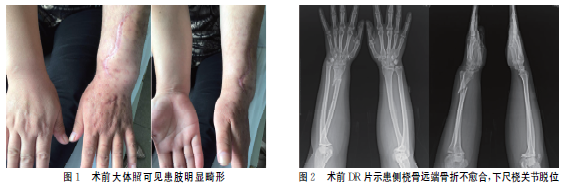
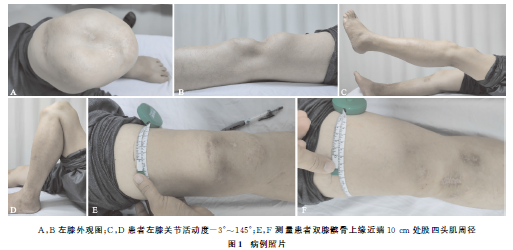
颞下颌关节脱位时间超过1个月,则可称为陈旧性颞下颌关节脱位(chronic prolonged mandibular dislocation,CPMD)。CPMD具有典型的病史和临床表现,其诊断并不困难,如果无法确诊可进行影像学检查。CPMD较少见,现报告1例超过6个月的CPMD手术治疗及效果。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#下颌#
82
#关节脱位#
65
#颞下颌#
71
#颞下#
66
#手术治疗#
66
#陈旧性#
67
#脱位#
76