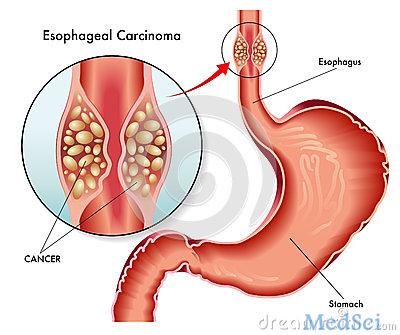
Journal of Clinical Gastroenterology:鳞状细胞癌抗原血清测定可以作为Barrett食管和食管癌的生物标记物:III期研究
2018-06-01 MedSci MedSci原创
目前Barrett食管(BE)的监测成本高居不下,仍然是临床难点之一,学界仍然不推荐在筛查和监测中使用生物标志物。因此为了评价鳞状细胞癌抗原的免疫复合形式的确定的潜在作用SCCA-immunoglobulin(Ig)作为筛选Barrett食管(BE)和食管腺癌(EAC)可行性进行了本项研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#AST#
59
#GAS#
52
#测定#
88
#Gastroenterol#
50
#细胞癌#
56
#标记物#
58
#III期研究#
63
#III#
57
#RET#
62
#Barrett#
85