JAMA Inter Med:华法林治疗中断后复发性静脉血栓栓塞、出血和死亡风险
2015-05-28 崔倩 译 MedSci原创
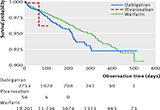
重要性 对于长期接受华法林钠治疗、预防继发性静脉血栓栓塞(VTE)的患者中,当他们需要为手术和侵入性诊断程序临时中断抗凝治疗的时候,出血和复发性VTE的风险还没有得到充分的说明。目的 为了描述那些采用华法林治疗的侵入性程序中断后和临床相关的出血和复发性静脉血栓栓塞概率,并比较那些接受和不接受搭桥治疗的患者的这些概率。 设计及参与者 &nb
过渡治疗在VTE患者中的过度使用:首先,不要伤害
美国约翰斯·霍普金斯大学布劳特曼(Brotman)和斯特雷夫(Streiff)在同期述评中指出,在因VTE而接受抗凝治疗的患者中,停用抗凝治疗时的复发风险存在较大差异。由于活动性血栓稳定之前停用抗凝的患者尤易出现栓塞,因此上次血栓事件时间可能为短期VTE复发的最重要决定因素。ACCP指南建议对因VTE病史接受抗凝治疗的患者进行分层:如果血栓形成发生在前3个月之内,则停用抗凝时复发为高危;在前3至12个月之间发生为中危;在12个月之前发生为低危。高凝状况亦可将患者分类为高危范畴。
近期研究强调了手术操作后全剂量应用抗凝治疗所导致的出血风险,在术后2至3天启动治疗时尤为显著。在此项研究中,仅三分之一的患者应用了过渡治疗,但却引发了14起增量临床相关性出血事件,其余三分之二未接受过渡治疗的患者仅发生3起血栓形成事件。尽管该研究效力不足以评估死亡率,但其他研究显示约10%的VTE患者因大出血死亡,相当于复发性VTE所致死亡率。
尽管此项研究存在未能区分全剂量和预防剂量抗凝过渡治疗,以及缺少抗凝治疗时机信息等局限之处,但亚组之间的出血和血栓形成事件不均衡情况可能较整体患者更为显著。大部分VTE抗凝患者无须接受治疗剂量过渡治疗。然而,一些复发性VTE高危患者仍需要应用过渡治疗,如1个月之内发生的急性VTE以及短期停用抗凝治疗后复发活跃患者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#复发性静脉血栓栓塞#
55
#治疗中断#
80
#复发性#
78
#静脉血#
80
#静脉#
71
看看
172
#死亡风险#
69
#Med#
62