冠心病支架术后的注意事项
2015-07-10 壹生 惠大夫在江湖
冠脉支架植入术(PCI术),是治疗冠心病的有力武器之一,能有效缓解心绞痛症状、挽救急性心肌梗死患者的生命。 但不少患者认为,支架植入是“根治性”手术,可以一劳永逸的解决冠心病,这是最常见的误区之一,因为支架术后还要继续进行常规的药物治疗及生活方式的管理,针对该问题,分三大方面跟大家详细分享一下。 一 遵医嘱服药 1.阿司匹林 如无不良反应及禁忌症,阿司匹林需要终身服用,可选用阿
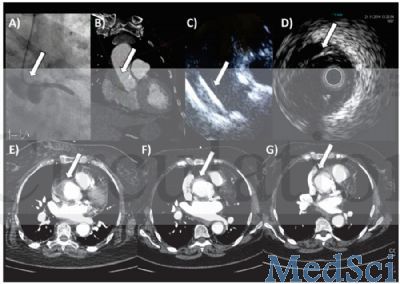
冠脉支架植入术(PCI术),是治疗冠心病的有力武器之一,能有效缓解心绞痛症状、挽救急性心肌梗死患者的生命。
但不少患者认为,支架植入是“根治性”手术,可以一劳永逸的解决冠心病,这是最常见的误区之一,因为支架术后还要继续进行常规的药物治疗及生活方式的管理,针对该问题,分三大方面跟大家详细分享一下。
一 遵医嘱服药
1.阿司匹林
如无不良反应及禁忌症,阿司匹林需要终身服用,可选用阿司匹林肠溶片(100mg/片)。
2.氯吡格雷(等)
术后一般都需要服用两种抗血小板药物,包括上述的阿司匹林,另一种还有目前常用的药物有氯吡格雷,及刚在我国上市的替格瑞洛。服用时间需要根据支架类型及患者病情等方面来定,一般要服用1年。
3.他汀类调脂药 如阿托伐他汀、瑞舒伐他汀
患者对该药存在严重的错误理解,很多人在检查血脂“正常”以后,就停止服药,大错而特错。冠心病患者血脂水平,和普通正常人是不同的,除非一些特殊情况,即使血脂在“正常”水平,也要长期服用此药,如血脂未达标,可能还需要增加药物剂量。
4.其它药物,如血管紧张素转换酶抑制剂(如“xx普利”),β受体阻断剂(如“倍他乐克”)
此类药物作为冠心病的基石性药物,作用不容忽视,特别是对于那些心肌梗死的患者,但不见得所有患者都需要或都能耐受,需遵医嘱服用。
二 定期随诊
一般术后2-3周第一次复诊,医生会根据患者的个体情况,复查相关化验检查,并调整药物的剂量。一定要注意,很多冠心病的用药剂量并非固定不变,如他汀类药物、血管紧张素转换酶抑制剂、β受体阻断剂等,请务必谨记。而且,每种药物都可能对机体产生副作用,要随诊监测,比如他汀类药物可能会引发肝酶升高等副作用。
三 生活管理
1.运动
每个手术患者对运动的耐受能力不同,和心脏功能、血管狭窄程度、支架开通情况等因素有关。有的患者术后活动量可以逐渐恢复至正常健康状态,而有的患者可能恢复不到原来的水平,而且需根据医生的建议逐渐恢复运动,不能短期内突然增加运动量。
2.饮食
基本遵循“低盐低脂”的原则,多食用新鲜蔬菜、水果、鱼肉、豆制品和奶制品等,不宜常吃或大量吃动物内脏及高脂肪、高胆固醇食物。限制饮酒,建议每日饮酒限量:白酒50ml,啤酒300ml,红酒100ml。
3.戒烟
戒烟,毋庸置疑。香烟不但能加速动脉粥样硬化进程,而且能直接导致冠脉损害、痉挛等。所以,不论是否罹患冠心病,都应该严格戒烟,包括二手烟。
4.控制体重
肥胖是“万恶之源”,高血压、糖尿病、高血脂,都可继发于肥胖。教大家一个估算自己是否肥胖的一个方法,计算体重指数(BMI),用体重(kg)/身高x身高(m),正常值为18.5-23.9,>24称为超重,>28称为肥胖,而第八版《内科学》上,已把>24称为“肥胖症”。您计算一下,如果超重,就赶紧减肥。
5.乐观的情绪、充足的睡眠
研究证明,大部分冠心病患者都各并心理问题,包括焦虑、抑郁等,而且,不良情绪可能会加重、诱发心肌缺血发作,所以,保持平稳、乐观的情绪尤为重要。同时,充足的睡眠会让您一天的精神满满,我个人建议至少保证7-8小时的睡眠。
6.监测血压、控制血糖
治疗冠心病,务必要同时控制血压、血糖,这些环节缺一不可。
综上建议,我相信,如果每个患者能切实履行,必会最大程度的维护健康、延缓疾病进展。当然,支架手术不能万能的,并不是所有冠心病患者都需要、或都能够进行支架植入治疗,手术前后需要专业医生进行评估,而且,支架手术,不是一劳永逸的,严格的药物治疗+支架植入,才是治疗冠心病的根本。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很浅显易懂,适合做成患者健康教育
87
#支架术#
58
#支架术后#
57
#注意事项#
58
冠心病患者科普!
130
没什么太大新价值
143
牛
152
看看
81
又学习了
77
很有用
106