Rapid Medical的DISTALS中风试验首位患者入组——为新发缺血性中风患者群体提供治疗
2022-06-07 网络 网络
TIGERTRIEVER™ 13为多中心关键性的DISTALS试验提供支持,是市面上仅有的为远端血管设计的超小型血栓切除器械
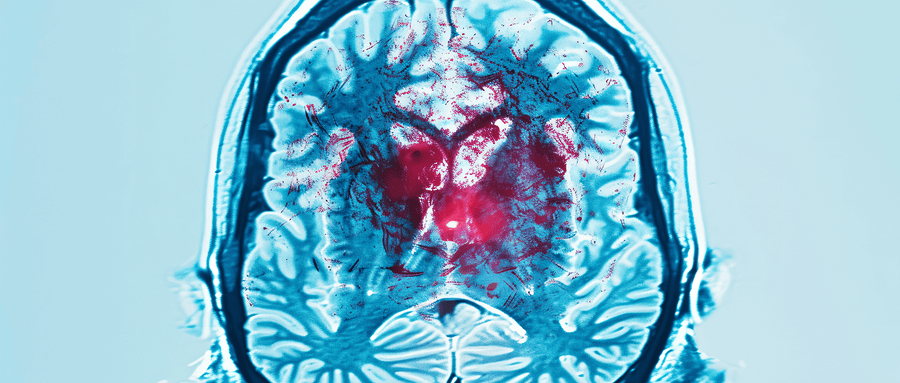
先进神经血管器械的领先开发商Rapid Medical今天宣布,DISTALS研究的首位患者已经入组。该试验是美国食品药品管理局(FDA)有史以来第一个研究机械血栓切除术在远端中风中的安全性和有效性的试验用器械豁免(IDE)试验。
德国索林根radprax Neurocenter神经放射科主任Hannes Nordmeyer博士表示:“第一位患者入组这项具有标志性意义的研究,对患者来说是一个重要的里程碑。我们从大血管缺血性中风中了解到,尽快恢复脑部血流可大大改善疗效。现在借助TIGERTRIEVER 13,我们有了触及远端中风的技术,我们必须理解快速打开较小血管对患者的好处。”
Rapid Medical的TIGERTRIEVER™13开创了缺血性中风的这一新领域。它是目前首屈一指的微型可调式血栓切除器械。凭借TIGERTRIEVER 13的可调节性和完全可视性,医生可以远程控制与血管和血栓的接触。这样一来,手术的每个步骤都得到优化。
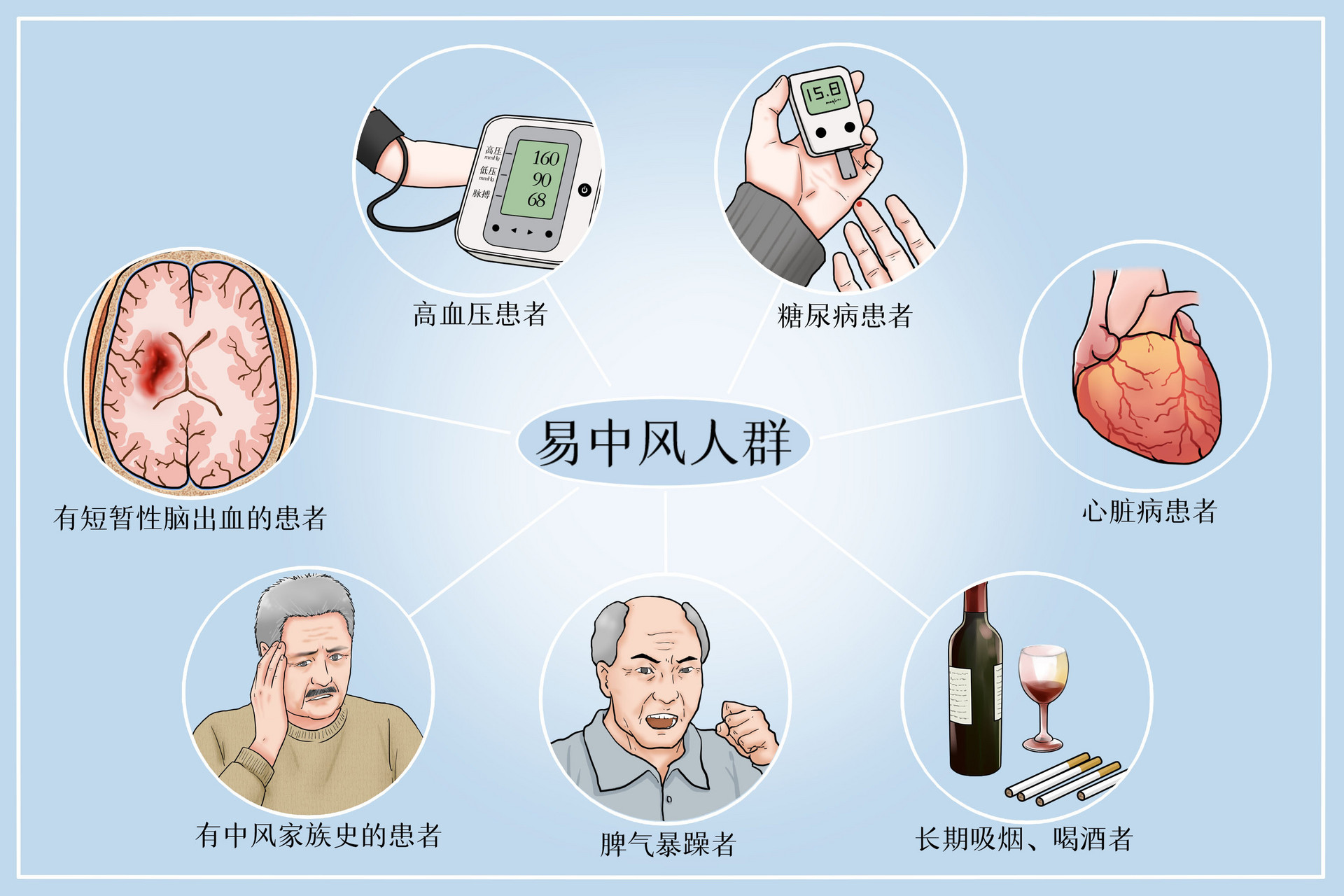
不到10%的缺血性中风患者会接受机械血栓切除术。这是一种可明显改善患者预后的成熟疗法。借助Rapid Medical的TIGERTRIEVER 13,DISTALS研究旨在将这些好处带给另外25 – 40%的中风患者。该研究专注于M3血管等外围大脑区域,并允许在症状发生后24小时内进行干预。
本新闻是与纽约市试验基地的首席研究员召开国际研究员会议之后发布的。与会者包括加州洛杉矶市加州大学洛杉矶分校的Jeffrey Saver博士;佐治亚州玛丽埃塔市Wellstar Health System的Rishi Gupta;纽约州石溪市石溪大学医疗中心的David Fiorella;以及德国埃森市Alfried Krupp Krankenhaus的René Chapot教授。在这次活动中,全球资深专家们讨论了治疗这一患者群体和优化手术程序的挑战。
Rapid Medical首席临床官Walid Haddad博士表示:“我们很高兴有这样一个强大的医师贡献团队来帮助推动这个领域。我们正在深入了解中风以及该器械的新颖设计如何在安全治疗这些脆弱的大脑区域方面发挥关键作用。”
除了德国的Hannes Nordmeyer博士入组的第一名患者外,纽约州立大学布法罗分校神经外科的Elad Levy博士刚刚入组了第一名美国患者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#缺血性#
68
#群体#
89
#Dis#
69
#首位患者#
80
#DIC#
63
#缺血性中风#
96
#Medical#
108
#中风患者#
66
#Med#
59