微生物所肠道菌群和炎症性肠病研究获进展
2017-03-07 佚名 微生物研究所
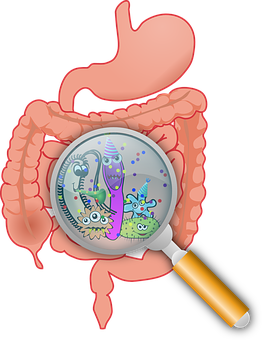
肠道菌群在人体健康中发挥着重要作用。近年来,有关肠道菌群的研究日益成为科学家们感兴趣的焦点。宿主和肠道菌群在长期的进化过程中相互作用,共同调节肠道内环境稳态,对这一“共生 - 互益”的复杂机制的探索将对研究因肠道菌群异常而引起的疾病的发病机制具有重要意义。
肠道菌群在人体健康中发挥着重要作用。近年来,有关肠道菌群的研究日益成为科学家们感兴趣的焦点。宿主和肠道菌群在长期的进化过程中相互作用,共同调节肠道内环境稳态,对这一“共生 - 互益”的复杂机制的探索将对研究因肠道菌群异常而引起的疾病的发病机制具有重要意义。
克罗恩病 (Crohn’s disease) 是一种危害人类健康的重大疾病。但是其病因及发病机制仍不十分明确。目前为止,越来越多的研究表明克罗恩病患者肠道菌群发生了明显变化,这一变化在克罗恩病的发病机制中起重要作用。

实验室下一步将重点研究肠道菌群在克罗恩病发病过程中的关键作用及其调控免疫反应的具体机制,这对推动克罗恩病的个性化治疗有重要的意义。
该项成果于近日在线发表于 Journal of Immunology 杂志上,张福萍课题组的助理研究员高平为文章的第一作者,该组的研究生刘宏涛和黄华镕等也参与了部分工作,张福萍为通讯作者。该研究得到国家自然科学基金(31300719 和 31470861)和国家重点研发计划项目(2016YFC1200302)的资助。
原始出处:Ping Gao, Hongtao Liu, Huarong Huang,et al.The Inflammatory Bowel Disease–Associated Autophagy Gene Atg16L1T300A Acts as a Dominant Negative Variant in Mice.J Immunol .February 15, 2017.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#微生物#
50
#研究获进展#
59
#肠道菌#
0
#炎症性#
48
肠道菌群火的一塌糊涂
56