Cell Stem Cell:首次在肝脏内将导致肝病的细胞转化为功能性的肝细胞
2016-06-06 佚名 生物谷
干细胞研究取得的进展使得在实验室培养皿中能够将病人的皮肤细胞转化为心脏细胞、肾脏细胞和肝细胞等,这就给科学家们提供希望:有朝一日,这些细胞能够替换器官移植用于治疗器官衰竭病人。但是将这些细胞成功地移植到病人的功能衰竭的器官中仍然是一个重要的临床挑战。如今,来自美国加州大学旧金山分校和德国海德堡大学医院的研究人员在小鼠体内证实在肝脏内产生健康的新的肝细胞是可能的,这就使得细胞移植是不必要的。

干细胞研究取得的进展使得在实验室培养皿中能够将病人的皮肤细胞转化为心脏细胞、肾脏细胞和肝细胞等,这就给科学家们提供希望:有朝一日,这些细胞能够替换器官移植用于治疗器官衰竭病人。但是将这些细胞成功地移植到病人的功能衰竭的器官中仍然是一个重要的临床挑战。
如今,来自美国加州大学旧金山分校和德国海德堡大学医院的研究人员在小鼠体内证实在肝脏内产生健康的新的肝细胞是可能的,这就使得细胞移植是不必要的。更重要的是,他们是将肝脏内导致肝病的细胞(即肌成纤维细胞)转化为健康的新的肝细胞,因而同时降低肝脏损伤和改善肝脏功能。论文通信作者、加州大学旧金山分校外科教授Holger Willenbring说,这一方法采用一种已在利用肝脏靶向基因疗法治疗病人中获得早期验证的病毒基因运送技术,这提示着它可能很容易进行临床转化,用于治疗肝病患者。相关研究结果发表在2016年6月2日那期Cell Stem Cell期刊上,论文标题为“In Vivo Hepatic Reprogramming of Myofibroblasts with AAV Vectors as a Therapeutic Strategy for Liver Fibrosis”。
Willenbring说,“该方法如此有效的部分原因是肝脏是一个具有自然再生能力的器官,因此它能够非常好地适应新的细胞。我们观察到转化后的细胞不仅在功能上整合进肝脏组织中,而且也能够分裂和增殖,从而导致新的肝脏组织块产生。”
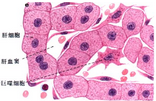
在美国,超过60万人遭受终末期肝病或肝硬化的折磨。唯一可用的治愈方法就是肝脏移植,但是供者肝脏短缺意味着在美国每年只有6***受益于这种疗法,而超过3.5万人因这种疾病死亡。 肝纤维化是肝脏渐进性形成瘢痕组织,是肝脏疾病的主要触发因子。当肝细胞不能够足够快速地再生而赶不上酒精等有毒物质或丙型肝炎或脂肪肝等疾病导致的损伤时,肝纤维化就产生了。肌成纤维细胞(myofibroblast)填充肝细胞死亡后留下的空隙,形成类似瘢痕组织的纤维化组织。
肝纤维化发展过程缓慢,但是能够导致严重的肝功能衰竭:一个人在25岁感染上丙型肝炎病毒(HCV),可能在几十年内感觉很好,然后在50岁时突然开始经历疲劳、昏眩、恶心、挫伤、腹泻和黄疸,这表明终末期肝病开始发作。原因在于只要肝脏有至少20%是功能性的,它就能适应,但是一旦它低于这一临界阈限,病人通常在两年内死亡。
在小鼠体内降低肝脏损伤和增加肝脏功能
Willenbring致力于利用干细胞生物学技术产生新的肝细胞(比如,由病人的皮肤细胞转化而来)以便能够替换组织移植来治疗肝脏衰竭。然而,未预料到的是,当Willenbring和他的实验室接近实现这一梦想时,他不得不意识到这种细胞疗法可能不能用于治疗绝大多数肝脏衰竭患者,这是因为肝脏内纠缠在一起的纤维化组织本身会破坏移植细胞的成功定植。
因此,在过去5年,Willenbring和他的团队与来自海德堡大学医院的Dirk Grimm博士及其团队密切合作,着手研究一种不同的方法:在肝脏内,将导致肝纤维化的肌成纤维细胞转化为健康的新的肝细胞。
之前的研究已鉴定出基因调节蛋白混合物能够将其他类型的细胞转化为肝细胞,但是研究人员需要一种方法将这些指令运送到肌成纤维细胞中。在多年的研究后,研究人员鉴定出一种腺相关病毒(adeno-associated virus, AAV)亚型AAV6能够特异地感染肌成纤维细胞。因此,研究人员着重关注AAV,这是因为已证实它在早前的人基因疗法临床试验中是安全的和有效的。
研究人员在肝病小鼠体内证实装填上改变细胞命运的混合物的AAV6确实感染肌成纤维细胞,并且将它们转化为功能性的肝细胞。新产生的肝细胞数量相对较少---不到接受治疗的小鼠体内所有肝细胞的1%,但是这仍然足以降低肝纤维化和改善肝脏功能。
研究人员说,在培养皿中,这种病毒方法也高效地将人肌成纤维细胞转化为功能性的肝细胞,但是还需要开展更多研究以便让这种方法也能用于病人体内。特别地,Willenbring实验室正在努力将这种方法中所使用的混合物包装到单个病毒中,以便降低潜在的副作用和简化临床开发。该实验室也正在努力将让AAV6病毒对肌成纤维细胞的特异性变得更强,这是因为在当前的这项研究中,该病毒也能够感染肌细胞和免疫系统中的一些细胞,不过不能将它们转化为肝细胞,而且也不会明显地影响它们的功能。
Willenbring说,这些新的结果提示着在发生纤维化的肝脏中,相比于细胞移植方法,这种方法可能能够更加高效地和稳定地改善肝脏功能,并且补充道,一旦病毒包装得到优化,这种疗法可能能够在众多医学机构中低成本地开展,而不仅仅是在能够开展干细胞移植的专科医院中开展。
Willenbring是第一个承认这种新技术并不能替换当前的标准肝病疗法:“肝脏移植仍然是最好的治疗选择。但是如果它能够将肝脏功能提高百分之几,那么这就有希望让病人的肝脏功能维持在临界阈值之上,而这可能意味着多活几十年。”
原始出处
Milad Rezvani9, Regina Español-Suñer9, Yann Malato9, Laure Dumont9, Andrew A. Grimm, Eike Kienle, Julia G. Bindman, Ellen Wiedtke, Bernadette Y. Hsu, Syed J. Naqvi, Robert F. Schwabe, Carlos U. Corvera, Dirk Grimm, Holger Willenbring.In Vivo Hepatic Reprogramming of Myofibroblasts with AAV Vectors as a Therapeutic Strategy for Liver Fibrosis.Cell Stem Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#stem cell#
89
#Cell#
45
#CEL#
40
#功能性#
47
#肝细胞#
61
#STEM#
45
好文章啊
133
需进一步研究
150