Cancer Cell:弥散性大B细胞淋巴瘤协同性化疗新进展
2012-06-18 bo 生物谷
6月12日,Cancer Cell杂志报道了弥散性大B细胞淋巴瘤化学协同治疗的最新进展。 癌基因突变的知识,可催生靶向性杀死癌细胞而避免正常细胞受害的治疗手段。来那度胺在弥散性大B细胞淋巴瘤(DLBCL)的活化B细胞样(ABC)亚型中是一种活性药物。由于ABC DLBCL细胞中存在MYD88癌基因,来那度胺可通过促进干扰素β (IFNβ)的产生来杀死这些癌细胞。 来那度胺以cereblon依赖

6月12日,Cancer Cell杂志报道了弥散性大B细胞淋巴瘤化学协同治疗的最新进展。
癌基因突变的知识,可催生靶向性杀死癌细胞而避免正常细胞受害的治疗手段。来那度胺在弥散性大B细胞淋巴瘤(DLBCL)的活化B细胞样(ABC)亚型中是一种活性药物。由于ABC DLBCL细胞中存在MYD88癌基因,来那度胺可通过促进干扰素β (IFNβ)的产生来杀死这些癌细胞。
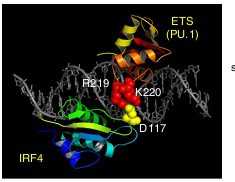
来那度胺以cereblon依赖的方式下调IRF4和SPIB的水平。这两个转录因子一起通过抑制IRF7和上调促生存的NF-kappa-B信号通路预防IFNβ的产生。利用Bruton 的酚基乙氨酸激酶(BTK) 抑制剂ibrutinib阻断B细胞受体信号,也可下调IRF4,并与来那度胺协同杀伤ABC DLBCL细胞。该研究表明,ibrutinib与来那度胺结合或可成为新的治疗策略。

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
Exploiting Synthetic Lethality for the Therapy of ABC Diffuse Large B Cell Lymphoma
Yibin Yang, Arthur L. Shaffer, N.C. Tolga Emre, Michele Ceribelli, Meili Zhang, George Wright, Wenming Xiao, John Powell
Knowledge of oncogenic mutations can inspire therapeutic strategies that are synthetically lethal, affecting cancer cells while sparing normal cells. Lenalidomide is an active agent in the activated B cell-like (ABC) subtype of diffuse large B cell lymphoma (DLBCL), but its mechanism of action is unknown. Lenalidomide kills ABC DLBCL cells by augmenting interferon β (IFNβ) production, owing to the oncogenic MYD88 mutations in these lymphomas. In a cereblon-dependent fashion, lenalidomide downregulates IRF4 and SPIB, transcription factors that together prevent IFNβ production by repressing IRF7 and amplify prosurvival NF-B signaling by transactivating CARD11. Blockade of B cell receptor signaling using the BTK inhibitor ibrutinib also downregulates IRF4 and consequently synergizes with lenalidomide in killing ABC DLBCLs, suggesting attractive therapeutic strategies.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
56
#cancer cell#
72
#CEL#
64
#细胞淋巴瘤#
82
#B细胞#
61