NEJM:皮肤色斑-案例报道
2016-12-01 xing.T MedSci原创
皮肤斑点,在休克病人中是较为常见的临床标志,是由于皮肤缺血导致暗紫色的皮肤变色。它最常出现的部位在膝盖周围,但也可以出现在耳朵和手指等部位。该患者被诊断为腺病毒导致的急性心肌炎并发心源性休克。
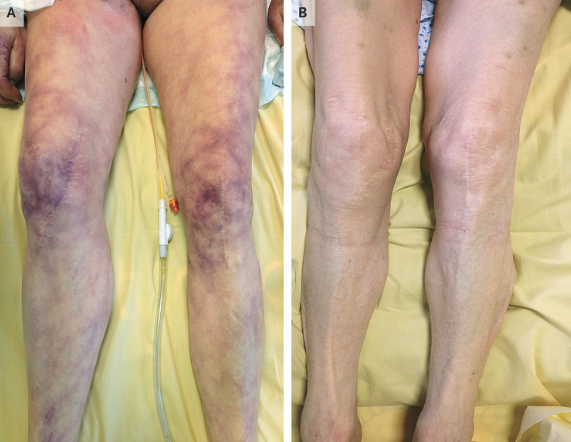
一名68岁的女性患者因呼吸衰竭和低血压被ICU收入院。入院时,该患者血压为70/50mmHg,心率为125次/分。体格检查发现患者大腿皮肤可见暗紫色斑纹(如图A)。实验室检查发现动脉血乳酸水平发生了明显变化为4.5mmol/L(正常值<2.0 mmol/L)、心脏肌钙蛋白T水平为0.43ng/mL(正常值<0.014 ng/mL)、N末端脑钠肽前体水平为24500 pg/mL(正常值<900 pg/mL),通过聚合酶链反应(PCR)检测支气管肺泡灌洗液和血液发现腺病毒阳性。没有发现其他病毒或细菌。经胸超声心动图显示左心室射血分数为25%。
皮肤色斑,在休克病人中是较为常见的临床标志,是由于皮肤缺血导致暗紫色的皮肤变色。最常出现的部位在膝盖周围,但也可以出现在耳朵和手指等部位。该患者被诊断为腺病毒导致的急性心肌炎并发心源性休克。
对该患者主要处理措施为支持治疗包括机械通气、血浆容量扩张和正性肌力药物治疗。该患者的皮肤色斑在治疗后24小时内消失(如图B),并且到治疗后第3天左室射血分数增加到60%,患者最终完全康复出院。
原始出处:
Damien Contou,et al. Skin Mottling. N Engl J Med.December 1, 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






挺好的案例。
83
讲的好,学习了,分享了
108
感谢分享经典案例
97
讲的好,分享了
105
这就要跨学科了
83
临床有时候还是得多想想
52